Unusual Presentation of Empyema Necessitans caused by Fusobacterium Infection
Received: 08-Sep-2024, Manuscript No. amhsr-24-147586; Editor assigned: 10-Sep-2024, Pre QC No. amhsr-24-147586 (PQ); Reviewed: 24-Sep-2024 QC No. amhsr-24-147586; Revised: 01-Oct-2024, Manuscript No. amhsr-24-147586 (R); Published: 08-Oct-2024
Citation: Singh I. Unusual Presentation of Empyema Necessitans caused by Fusobacterium Infection. Ann Med Health Sci Res. 2024; S3:1-3.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Empyema necessitans is a rare complication of pleural empyema with extension of the empyema outside the pleural space into the neighbouring chest wall and surrounding soft tissues. Most cases occur as a result of inadequately treated empyema related to necrotizing pneumonia or lung abscess. Mycobacterium tuberculosis and Actinomyces are the most common pathogens isolated from empyema necessitans. We are reporting in this article a rare case of Chronic Obstructive Pulmonary Disease (COPD) patient presented with unresolving pneumonia and found to have pleural effusion extended to the chest and abdominal wall. Images and fluid analysis confirm the diagnosis of empyema necessitans caused by Fusobacterium infection and the patient was improved significantly after fluid drainage and culture sensitive antibiotic treatment.
Keywords
Empyema necessitatis; Interventional pulmonology; Chest wall abscess; Diagnostic thoracocentesis; Severe pneumonia; Fusobacterium infection
Introduction
Empyema refers to the macroscopic detection of purulent pleural fluid and represents one end of a spectrum of pleural infections which include empyema and complicated parapneumonic effusion. Most community-acquired pleural infections are caused by gram-positive aerobic organisms, especially streptococcal species. Gram-negative bacteria can also be a contributing factor but to a lesser extent. In contrast, hospital acquired pleural infection is dominated by resistant gram-positive organisms (including Methicillin-Resistant Staphylococcus aureus (MRSA)) and gram-negative organisms such as Escherichia coli, Enterobacter and Pseudomonas [1,2].
Empyema necessitans commonly occurs when an empyema extends into the surrounding subcutaneous tissues of the chest wall but can also spread to involve other sites such as the oesophagus, breast, retroperitoneal, peritoneal, pericardial and paravertebral regions [2].The resultant subcutaneous abscess may rupture through the skin.
Mycobacterium tuberculosis and Actinomyces species are thought to be the most common organisms causing empyema necessitans. However, there are reported cases of empyema necessitans caused by other microorganisms such as Blastomycosis, Aspergillus, Nocardia, Mucormycosis and Fusobacterium [3,4].
Case Presentation
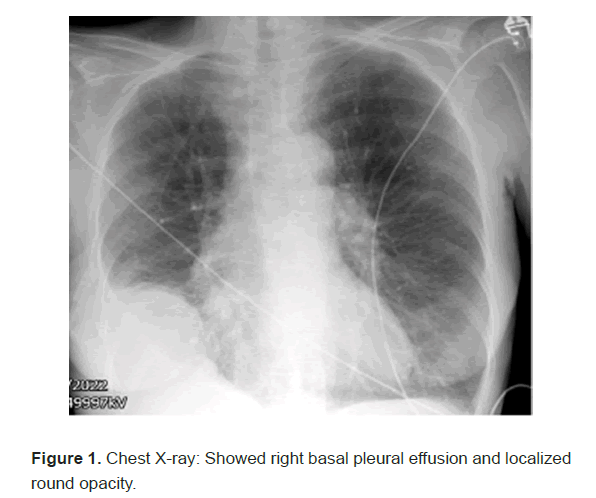
A 60 year old female with a medical history of osteoporosis, lumbar spondylosis and advanced Chronic Obstructive Pulmonary Disease (COPD) on Long Term Oxygen Therapy (LTOT) at two litres daily for 16 hours, presented to the emergency department with worsening shortness of breath over several weeks. She had undergone two courses of rescue antibiotics (doxycycline) and prednisolone, followed by a third course prescribed by her general practitioner, with minimal improvement. There was no history of cough or fever. On examination she found to have a dental swelling. Chest-Xray showed the right basal pleural effusion and localized round opacity (Figure 1).
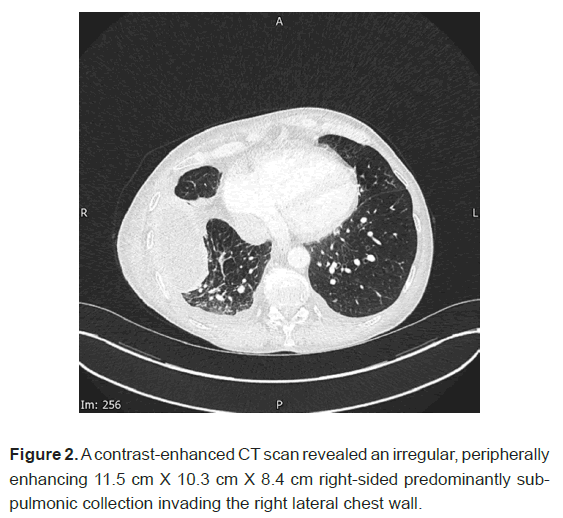
A contrast enhanced Computed Tomography (CT) scan revealed an irregular, peripherally enhancing 11.5 cm Χ 10.3 cm Χ 8.4 cm right-sided predominantly sub-pulmonic collection invading the right lateral chest wall (Figure 2).
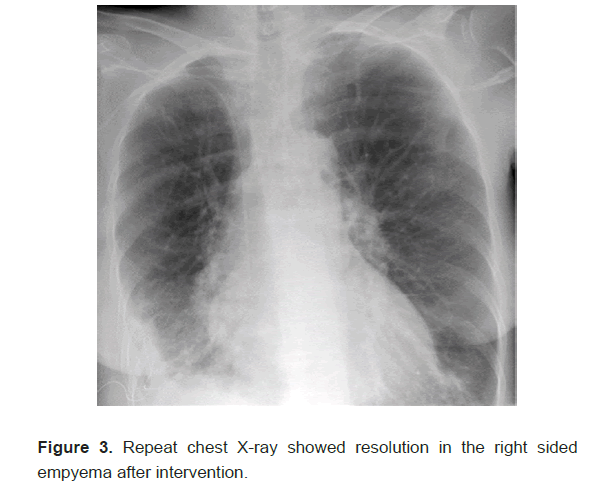
A thoracocentesis was performed which yielded 350 mls of thick foul smelling pus, with cultures showing a heavy growth of Fusobacterium species. The patient was escalated to meropenem following microbiology advice. Lemierre syndrome was also considered due to dental swelling, but was later ruled out as no specific radiological signs of dental abscess were founds and the CT scan showed no evidence of jugular vein thrombosis. As the empyema was localized and was difficult to be drained by the simple aspiration, CT guided chest drain inserted with the help of the interventional radiologist. Fluid drained effectively and repeated chest X-ray showed reduction in the empyema (Figure 3). Due to persistent tachypnoea and CO2 retention, the patient was kept on Non-Invasive Ventilation (NIV) and was seen by palliative team who adjusted her symptomatic treatment for the dyspnoea and she was discharged on NIV and course of antibiotic. Subsequent follow-up indicates significant recovery of the empyema and she continued on regular use of NIV and LTOT.
Results and Discussion
Pleural infection represents a significant medical issue, characterized by substantial morbidity and mortality rates. 20% of patients dying after an episode of pleural infection over 12 months and the requirement for surgery in around 15%. The incidence of pleural infection in United Kingdom (UK) reported to be around 11.2 cases per 100,000 population per year. Recent data from the UK show an increase in the rate of pleural infections, particularly among the elderly population; however, the cause of this increased rate remains unclear. Empyema refers to the macroscopic detection of purulent pleural fluid and represents one end of a spectrum of pleural infection which include empyema and complicated parapneumonic effusion. The majority of community acquired pleural infections are attributed to gram-positive aerobic bacteria, predominantly streptococcal species. Gram-negative bacteria are less frequently isolated in cases of community acquired infections. In contrast, hospital acquired pleural infection is dominated by resistant gram-positive organisms (including Methicillin-Resistant Staphylococcus aureus (MRSA)) and gram-negative organisms such as Escherichia coli, Enterobacter and Pseudomonas [1].
Empyema progresses through three stages namely, the exudative stage, the fibrinopurulent stage and the organizing stage [5]. In the organization stage an inelastic membrane will be formed, which may encase the lung and restrict normal ventilatory function. If left untreated, the fluid may erode and spontaneously drain through the chest wall, a condition known as empyema necessitans and may also extend to other areas such as the oesophageal, breast, retroperitoneal, peritoneal, pericardial and paravertebral regions [2].The resulting subcutaneous abscess can ultimately rupture through the skin and lead to sepsis and multiple organ system failure. The clinical syndrome of empyema necessitans has become rare in modern clinical practice, thanks to advancements in antibiotic therapy and surgical techniques. It typically occurs in patients who have limited access to healthcare or are hesitant to seek appropriate medical care.
Mycobacterium tuberculosis and Actinomyces species are considered the most common organisms causing empyema necessitans. However, there are reported cases of empyema necessitans caused by other organisms such as Blastomycosis, Aspergillus, Nocardia, Mucormycosis and Fusobacterium [3,4].
A CT chest scan is the optimal radiological method for evaluating the extent of empyema necessitans, typically revealing a well demarcated collection that extends through the chest wall into an adjacent compartment. Destruction of nearby ribs may also be observed [6]. The treatment of empyema necessitans typically includes either closed or open drainage of the pleural space, which helps prevent fibrosis and allows the lung to expand. Administering the appropriate antibiotic therapy is also important in treating empyema necessitans [7]. In our case report we discuss a patient who is known to have severe COPD on LTOT who presented with unresolving pneumonia not responding to multiple courses of oral antibiotics. She also complains of chest wall and abdominal swelling and the CT confirmed presence of localized pleural effusion extending to the chest wall. Pleural aspirate was thick pus fluid and culture confirmed growth of Fusobacterium. Patient improved clinically and radiologically with sensitive antibiotic and CT guided chest drain.
Conclusion
Empyema necessitans is a complication of empyema that arises from delayed treatment, spreading to the surrounding chest wall and soft tissue. While Mycobacterium tuberculosis and Actinomyces are the most common pathogens, other organisms are also reported in the literature, as reported in this case, can also cause empyema necessitans. The patient responded well to an antibiotic regimen tailored to sensitivity results, along with fluid drainage. Despite the low incidence of empyema necessitans, we aim to raise physician awareness through this case report and emphasize the importance of monitoring and following up pneumonia cases to prevent progression. As empyema necessitans arise from complicating pneumonia and empyema, it is important for physicians to aggressively treat any complicating pneumonia. They should consider diagnostic pleural aspiration with a low threshold and consult with an infectious disease specialist regarding antibiotic selection. Additionally, early discussion with a surgeon about potentially complicating pleural procedures may be necessary to prevent the progression of pneumonia to empyema necessitans.
References
- Rahman NM, Chapman SJ, Davies RJ. The approach to the patient with a parapneumonic effusion. Clin Chest Med. 2006; 27(2):253-266.
- George RB, Light RW, Matthay MA. Diseases of the pleura, mediastinum, chest wall and diaphragm, chest medicine: Essentials of pulmonary and critical care medicine.1990; 4:441-477.
- Bhatt GM, Austin HM. CT demonstration of empyema necessitatis. J Comput Assist Tomogr. 1985; 9(6):1108-1109.
- Hockensmith ML, Mellman DL, Aronsen EL. Fusobacterium nucleatum empyema necessitans. Clin Infect Dis. 1999; 29(6):1596-1598.
- Hassan M, Patel S, Sadaka AS, Bedawi EO, Corcoran JP, et al. Recent Insights into the management of pleural infection. Int J Gen Med. 2021; 14:3415-3429.
- Weerakkody Y, Sharma R, Niknejad M. Empyema necessitans. Radiopaedia.2024.
[Crossref]
- Asciak R, Bedawi EO, Bhatnagar R, Clive AO, Hassan M, et al. British Thoracic Society Clinical Statement on Pleural Procedures. Thorax. 2023; 78(Suppl3):s43-s68.




 The Annals of Medical and Health Sciences Research is a bi-monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a bi-monthly multidisciplinary medical journal.