Use of Anti-shock Trousers during Surgery of the Posterior Fossa in the Sitting Position
Citation: Houba A, et al. Use of Anti-shock Trousers during Surgery of the Posterior Fossa in the Sitting Position. Ann Med Health Sci Res. 2018;8:103-104
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Letter to Editor
The lesions of the posterior fossa can be addressed by different surgical positions. Recourse to sitting still varies according to the different neurosurgical centers. This position is especially suitable for the median lesions. It runs the risk of hypotension and air embolism. The latter remains the most feared complication challenging the anesthesiologists. To reduce these risks, various prevention methods exist such as intravenous fluids, the use of positive end-expiratory pressure and the use of an anti-shock trouser. The authors report the use of anti-shock trousers during surgery of the posterior fossa seated position. Written informed consent was obtained from the patient to publish this report.
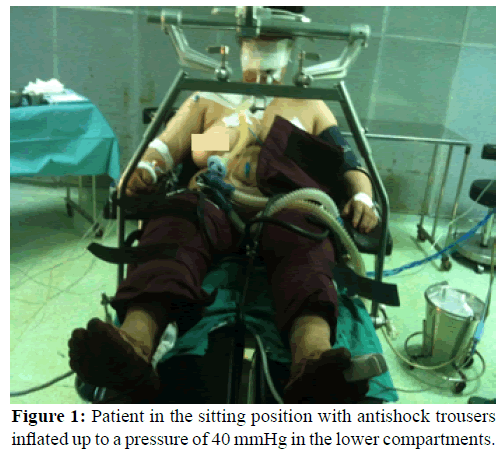
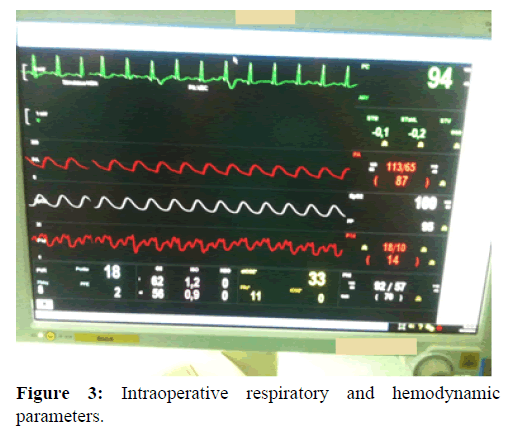
A 51-year-old female patient, with no other obvious abnormality, who was scheduled in our hospital for surgery of the posterior cerebral fossa in the sitting position. In the operating room, after securing venous access and routing monitoring including noninvasive arterial pressure, electrocardiography (ECG), and arterial saturation of oxygen by pulse oximetry (SpO2), an anti-shock pant with its three compartments (lower limbs and abdominal compartment) was performed. General anesthesia was induced with fentanyl (5 μg/kg), propofol (3 mg/kg). Orotracheal intubation was performed with a 7 mm endotracheal cuffed tube after inducing neuromuscular block with cisatracurium (0.15 mg/kg). Controlled volume ventilation was then commenced and the ventilator settings were adjusted to maintain a stable ETCO2 at 35-40 mmHg. A central venous catheter is inserted percutaneously via the right internal jugular vein, a radial artery is cannulated for invasive monitoring of arterial pressure, and hourly urine output via an indwelling bladder catheter. After induction the lower limb compartments were inflated up to a pressure of 40 mmHg followed by a vascular filling with 0.9% saline (1000 ml). The patient installation to a sitting position was done gradually [Figures 1 and 2] aiming to keep the knees at the level of the heart and with hips and knees flexed to aid venous return and minimize distention of the sciatic nerve. Anesthesia was maintained with isoflurane (1,5-2 MAC) and a mixture of air-oxygen. After stabilization, an 8 cm H2O PEEP was introduced. Continuous monitoring of end-tidal carbon dioxide throughout (ETCO2) was used to detect VAE. No signs of marked VAE were detected during the entire operation. All parameters remained stable with mean arterial pressure between 85 mmHg and 92 mmHg, central venous pressure between 12 and 14 cm H2O, capnography (ETCO2) between 34 and 38 mmHg and oxygen saturation over 98% [Figure 3]. After surgery, the anti-shock trouser was deflated. The duration of the operation was 4 hours, 5 minutes. The intraoperative blood loss was 400 ml and immediate postoperative period was uneventful. [1]
In posterior fossa surgery while sitting, air embolism remains a serious complication with a significant challenge for anaesthetists. All means of effective prevention must be undertaken to avoid this complication. [2,3] Among these means, we can mention the anti-shock pants that are the subject of our observation, but it is not used routinely in our practice. This consisted of a selfcontained unit, which is made up of one abdominal compartment and two leg compartments attached to an inflation unit. The anti-shock trousers is wrapped around the patient and inflated with compressed air to a pressure of 30-40 mmHg beginning with the lower limb compartments. The abdominal compartment was then inflated with a special attention to vital signs. Antishock trousers pressures were controlled continuously by the manometers integrated in the device. The procedure of deflation should be practiced slowly in one compartment at a time starting with the abdominal compartment. [4] Unfortunately, the use of positive end expiratory pressure (PEEP) during surgery proved to be not only ineffective, but also dangerous. At high PEEP, the effect on intrasinusal pressure appeared to be inverse. In addition, the incidence of VAE was not decreased by PEEP compared with conventional ventilation. However, the inflation of anti-shock trousers, when used in sitting position, induces an immediate elevate in right atrial pressure (RAP) and central venous pressure that is transmitted to the dural sinus. [4] This simple device has also been reported to be more effective in producing increases in RAP than 10 cm H2O of PEEP. [5]
The benefits of using anti-shock trousers must be weighed against the potential risks of decreasing vital capacity by 14%, hypoperfusion to intraabdominal organs, and compartment syndromes with incorrect inflation-deflation sequences. [2] In these cases, its routine use in patients with preexisting respiratory and cardiac disease cannot be fully justified.
Acknowledgements
The authors thank the team of Department of Anesthesiology and critical care at Military Hospital Mohammed V for providing support and helping in the preparation of the manuscript.
Funding
The building and writing of this article has not funding’s sources.
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- Porter JM, Pidgeon C, Cunningham AJ. The sitting position in neurosurgery: A critical appraisal. Br J Anaesth. 1999;82:117-128.
- Palmon SC, Moore LE, Lundberg J, Toung T. Venous air embolism: A review. J Clin Anesth 1997;9:251-257.
- Domaingue CM. Anaesthesia for neurosurgery in the sitting position: A practical approach. Anaesth Intensive Care. 2005;33:323-331.
- Meyer PG, Cuttaree H, Charron B, Jarreau MM, Perie AC, Sainte-Rose C. Prevention of venous air embolism in paediatric neurosurgical procedures performed in the sitting position by combined use of MAST suit and PEEP. British Journal of Anaesthesia 1994;73:795-800.
- Tassani P, Eberl-Lehmann P, Enzenbach R. Interatrial pressure difference during inflation of pneumaticantishock garments and positive end-expiratory pressure ventilation. J Neurosurg Anesthesiol. 1992;4:160-166.





 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.