Usefulness of Magnetic Resonance Imaging in the Diagnosis of Non-Alcoholic Wernicke’s Encephalopathy
- *Corresponding Author:
- Sohoni CA
Department of Radiology, NM Medical, Pune, Maharashtra, India
E-mail: sohonica@gmail.com
Abstract
A 38-year-old normotensive, non-diabetic, non-alcoholic male patient presented with altered sensorium and three episodes of generalized tonic clonic seizures in the past 3 days. Patient had undergone a right hemicolectomy and chemotherapy for cecal carcinoma 3 years ago, followed by excision of recurrent ileo-colic mass 2 years ago. Patient had received repeat chemotherapy 4 months ago for peritoneal metastatic disease, which had induced severe vomiting and diarrhea. He was on parenteral nutrition since then. On examination, the patient was obtunded, afebrile, pale, anicteric with stable vitals. He had bilateral decerebrate posture, was unresponsive to verbal commands and opened eyes only to a painful stimulus. Bilateral extensor plantar response and ankle clonus were elicited.
Sir,
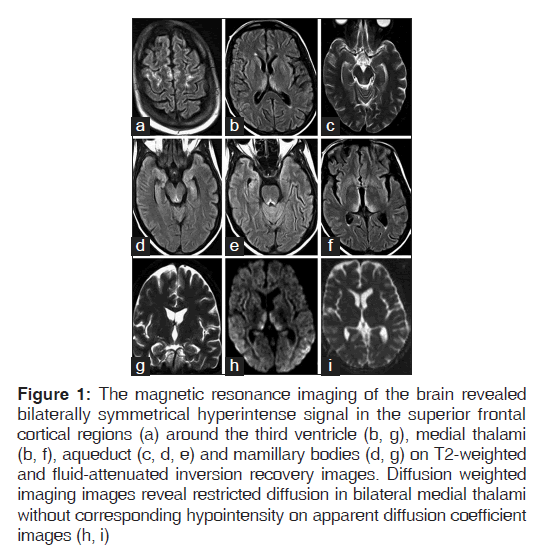
A 38-year-old normotensive, non-diabetic, non-alcoholic male patient presented with altered sensorium and three episodes of generalized tonic clonic seizures in the past 3 days. Patient had undergone a right hemicolectomy and chemotherapy for cecal carcinoma 3 years ago, followed by excision of recurrent ileo-colic mass 2 years ago. Patient had received repeat chemotherapy 4 months ago for peritoneal metastatic disease, which had induced severe vomiting and diarrhea. He was on parenteral nutrition since then. On examination, the patient was obtunded, afebrile, pale, anicteric with stable vitals. He had bilateral decerebrate posture, was unresponsive to verbal commands and opened eyes only to a painful stimulus. Bilateral extensor plantar response and ankle clonus were elicited. There was no neck stiffness and pupils were equally reactive to light. Horizontal nystagmus was seen on the 2nd day of hospitalization. Significant laboratory findings included a low hemoglobin of 7.6 g/dL, low platelet count of 36,000 and elevated serum creatinine of 4.8 mg/dL. The levels of serum vitamin B1 and B12 were within the normal limits. The magnetic resonance imaging (MRI) of the brain revealed bilaterally symmetrical hyperintense signal in the superior frontal cortical regions (a) around the third ventricle (b, g), medial thalami (b, f ), aqueduct (c, d, e) and mamillary bodies (d, g) on T2-weighted (T2W) and fluid-attenuated inversion recovery (FLAIR) images. Restricted diffusion was seen in bilateral medial thalami on diffusion imaging without corresponding hypointensity on apparent diffusion coefficient images (h, i) [Figure 1]. On the basis of clinical examination and MRI findings, a diagnosis of Wernicke’s encephalopathy (WE) was strongly suspected in spite of normal serum vitamin B1 levels. Patient was started on IV thiamine 100 mg daily for 5 days. Patient showed remarkable improvement in the level of consciousness within 24 h of the first dose. Complete resolution of all the neurological symptoms and signs was seen over the next 5 days and patient was subsequently discharged. WE is a life threatening medical emergency caused by thiamine deficiency, recognized primarily among alcoholics. The predisposing factors for this disorder among non-alcoholics include prolonged therapeutic fasting, total parenteral nutrition, hyperemesis gravidarum, gastrointestinal surgical procedures and chemotherapy among others. Cancer patients actively treated with chemotherapy may be particularly vulnerable.[1]
Figure 1: The magnetic resonance imaging of the brain revealed bilaterally symmetrical hyperintense signal in the superior frontal cortical regions (a) around the third ventricle (b, g), medial thalami (b, f), aqueduct (c, d, e) and mamillary bodies (d, g) on T2-weighted and fluid-attenuated inversion recovery images. Diffusion weighted imaging images reveal restricted diffusion in bilateral medial thalami without corresponding hypointensity on apparent diffusion coefficient images (h, i)
It requires a high index of suspicion to diagnose non-alcoholic WE which still remains underestimated because of either a relatively non-specific clinical presentation or poorly recognized clinical symptoms and signs.[2] The clinical diagnostic criteria for WE requires 2 of the following 4 signs: Dietary deficiencies, oculomotor abnormalities, cerebellar dysfunction and either an altered mental state and mild memory impairment.[3] Autopsy studies have revealed that approximately 75-80% cases of non-alcoholic WE in adults and 58% cases in children have been missed by routine clinical examination.[4]
WE is still diagnosed according to the history of the disease and therapeutic effect of thiamine supplementation. Theoretically, the determination of blood transketolase activity and thiamine phosphate or pyrophosphate can reflect the status of thiamine existing in the human body and be an accurate index in the diagnosis of WE.[5] However, no study has clearly described the sensitivity, specificity and accuracy of thiamine levels in relation to active disease. In our case, the normal levels of serum vitamin B1 were misleading. MRI is helpful in making a definitive diagnosis of WE, though the absence of findings does not rule it out.[6] The sensitivity of MRI is 53%, whereas the specificity is 93%.[6] Some case studies have reported that typical MR findings in WE include increased T2W and FLAIR signals symmetrically surrounding the aqueduct and third ventricle, at the floor of the fourth ventricle, in the medial thalami,[7,8] which is consistent with the MR findings in our patient. A few studies have reported atypical MR manifestations in the form of cortical involvement, which was also present in our patient.[9] Thus, the history, clinical findings, typical MR imaging features and response to thiamine administration allowed us to make a conclusive diagnosis of WE.
References
- Kuo SH, Debnam JM, Fuller GN, de Groot J. Wernicke’s encephalopathy: An underrecognized and reversible cause of confusional state in cancer patients. Oncology 2009;76:10-8.
- Sechi G, Serra A. Wernicke’s encephalopathy: New clinical settings and recent advances in diagnosis and management. Lancet Neurol 2007;6:442-55.
- Caine D, Halliday GM, Kril JJ, Harper CG. Operational criteria for the classification of chronic alcoholics: Identification of Wernicke’s encephalopathy. J Neurol Neurosurg Psychiatry 1997;62:51-60.
- Vasconcelos MM, Silva KP, Vidal G, Silva AF, Domingues RC, Berditchevsky CR. Early diagnosis of pediatric Wernicke’s encephalopathy. Pediatr Neurol 1999;20:289-94.
- Nordentoft M, Timm S, Hasselbalch E, Roesen A, Gammeltoft S, Hemmingsen R. Thiamine pyrophosphate effect and erythrocyte transketolase activity during severe alcohol withdrawal syndrome. Acta Psychiatr Scand 1993;88:80-4.
- Antunez E, Estruch R, Cardenal C, Nicolas JM, Fernandez- Sola J, Urbano-Marquez A. Usefulness of CT and MR imaging in the diagnosis of acute Wernicke’s encephalopathy. AJR Am J Roentgenol 1998;171:1131-7.
- Gallucci M, Bozzao A, Splendiani A, Masciocchi C, Passariello R. Wernicke encephalopathy: MR findings in five patients. AJNR Am J Neuroradiol 1990;11:887-92.
- Chung SP, Kim SW, Yoo IS, Lim YS, Lee G. Magnetic resonance imaging as a diagnostic adjunct to Wernicke encephalopathy in the ED. Am J Emerg Med 2003;21:497-502.
- Doss A, Mahad D, Romanowski CA. Wernicke encephalopathy: Unusual findings in nonalcoholic patients. J Comput Assist Tomogr 2003;27:235-40.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.