Why are Children Still Being Infected with HIV? Impact of an Integrated Public Health and Clinical Practice Intervention on Mother‑to‑Child HIV Transmission in Las Vegas, Nevada, 2007–2012
- *Corresponding Author:
- Dr. Ezeanolue EE
Department of Pediatrics, University of Nevada School of Medicine, 2040 W Charleston Blvd., Suite 402, Las Vegas, NV 89102, US.
E-mail: eezeanolue@medicine.nevada. edu
Citation: Ezeanolue EE, Pharr JR, Hunt A, Patel D, Jackson D. Why are children still being infected with HIV? Impact of an integrated public health and clinical practice intervention on motherto- child HIV transmission in Las Vegas, Nevada, 2007?2012. Ann Med Health Sci Res 2015;5:253-9.
Abstract
Background: During a 9 months period, September 2005 through June 2006, Nevada documented six cases of pediatric HIV acquired through mother‑to‑child transmission. Subsequently, a community‑based approach to the care of women and children living with or exposed to HIV was implemented. Subjects and Methods: A detailed review of mother‑infant pairs where HIV transmission occurred was performed to identify missed opportunities for prevention of mother‑to‑child HIV transmission. An intervention program was developed and implemented using the six‑step process. Data were collected prospectively over a 6 years period (2007–2012) and were evaluated for six core outcomes measures: (1) adequacy of prenatal care (2) HIV diagnoses of expectant mothers prior to delivery (3) appropriate use of antiretroviral (ARV) therapy before delivery (4) appropriate use of cesarean section for delivery (5) adequacy of zidovudine prophylaxis to newborn (6) HIV transmission rate. Results: Twenty‑six infants were born to HIV‑infected mothers from July 2005 to June 2006 with 6 documented infections. One hundred and five infants were born to HIV‑infected mothers from January 2007 to December 2012. Postimplementation, adequacy of prenatal care increased from 58% (15/26) to 85% (89/105); appropriate use of ARV therapy before delivery increased from 73% (19/26) to 86% (90/105); cesarean section as the method for delivery increased from 62% (16/26) to 74% (78/105); adequacy of zidovudine prophylaxis to newborn increased from 54% (14/26) to 87% (91/105). HIV transmission rate dropped from 23% (6/26) to 0%. Conclusion: Integrating public health and clinical services in the care of HIV‑infected pregnant women and exposed infants leads to better coordination of care and improved quality of care.
Keywords
HIV transmission, Implementation, Mother‑to‑child, Primary care, Public health
Introduction
Perinatal transmission of HIV can occur in utero, during delivery and postpartum through breastfeeding. The risk of perinatal HIV transmission depends on factor such as maternal viral load, infant mode of delivery, the presence of other sexually transmitted infections, and duration of ruptured membranes.[1‑3]
The risk of HIV transmission from an infected mother to a child varies from 15% to 30%.[4] This risk can be reduced to < 2% with appropriate intervention using combination antiretroviral (ARV) therapy during pregnancy and labor, delivery through cesarean section for HIV‑infected mothers with unknown viral load or viral load >1000 copies/ml and avoidance of breastfeeding among HIV‑infected women.[3] This has resulted in a dramatic decline in the number of children with perinatal HIV infection from an estimated annual peak of 1650 infected infants in mid‑1990s to 142 infants in 2005 in the United States.[5‑8] The framework for the elimination of perinatal transmission of HIV starts with the early identification of pregnant women who are HIV‑infected. Initially, the recommendation was targeted HIV screening of pregnant women, which was eventually changed to routine screening for all pregnant women in the United States.[9,10]
Nevada documented its highest cases of perinatally acquired HIV infection with eight confirmed cases in 1998 and was identified by the Centers for Disease Control and Prevention (CDC) as the only state west of the Mississippi River with an increasing number of women of childbearing age living with HIV infection in 2004.[11,12] Although Nevada had the nation’s 35th largest population at the time, it ranked 14th in the nation for the rate of adolescents/adults living with AIDS.[13] Six new cases of perinatally acquired HIV infections were documented in Clark County over a 9 months period from September 2005 to June 2006.[14] Clark County comprises the southern tip of Nevada and includes the cities of Las Vegas, Henderson, North Las Vegas and Boulder City.
The Department of Pediatrics at the University of Nevada‑School of Medicine received a Community Access to Child Health (CATCH) grant from the American Academy of Pediatrics (AAP) to determine why children were still being infected with HIV in Clark County. The medical records of HIV‑infected pregnant women who delivered an infant from July 2005 to June 2006 were reviewed, and common systemic barriers to prevention were identified.[15] Subsequently, funding from the Sawyer Foundation was utilized to develop and implement an intervention program based on the six‑step process developed by the Quality Enhancement Research Initiative (QUERI) of the Department of Veteran Affairs (VA) was received.[16] The program integrated public health services provided by the county health department (Southern Nevada Health District [SNHD]) with clinical care for HIV‑infected pregnant women and HIV‑exposed infant provided by a county hospital and the medical school, with a focus to reduce or eliminate mother‑to‑child transmission (MTCT) of HIV. This report summarizes the process and outcome of the integrated program. The institutional review boards of University of Nevada, Reno and the University Medical Center of Southern Nevada (UMC) approved this project.
Subjects and Methods
Subjects
Approximately 72% of the population in Nevada and 87% of people infected with HIV live in Clark County.[17] The Wellness Center at the UMC provides medical care to the majority of adults with HIV including women in Clark County. The Nevada Care Program at the University of Nevada School of Medicine (UNSOM) provides care to pregnant women and HIV‑exposed and infected children in Clark County. The SNHD provides surveillance and case management for HIV‑infected persons and Aid for AIDS of Nevada provides social services for individuals infected with HIV in Clark County.
Methods
The method was based on the principles of implementation science developed in 1998 by the VA QUERI and community‑based participatory research.[16] The six‑step approach includes: (a) identify a high burden clinical issue (b) identify evidence‑based clinical practice guidelines (c) define existing practices and identify performance gaps (d) develop and implement an intervention (e) evaluate system improvement (f) evaluate health outcomes and disseminate findings.
Identify a high burden clinic issue
The confidential name‑based HIV reporting system that was established in 1992 and is maintained by the SNHD was reviewed to identify HIV‑infected women of childbearing age. Data were extracted on women who delivered an infant between July 2005 and June 2006, and their prenatal and hospital delivery records were reviewed. The medical records of HIV‑exposed infants maintained by the UNSOM Department of Pediatrics were also reviewed. Data and medical record reviews were performed by a pediatric infectious disease specialist with expertise in the care of patients with HIV, who was assisted by a trained program coordinator.
Identify evidence‑based clinical practice guidelines
The medical literature was reviewed to identify current evidence‑based guidelines and recommendation in 2006, to reduce MTCT including those from the CDC, American College of Gynecologist, AAP; United States Preventive Services Task Force (USPSTF) and the Institute of Medicine (IOM).[18‑21] All of the above agencies identified routine prenatal HIV testing as a rate‑limiting step toward prevention of mother‑to‑child HIV transmission (PMTCT) and lack of corrdination of care as creating missed opportunities for preventing MTCT. HIV‑infected pregnant women identified early in pregnancy who are able to be enrolled in prenatal care and have access to available ARV therapy are shown to reduce significantly the risk of HIV transmission. HIV‑infected pregnant women identified during labor are still able to reduce the risk of transmission to < 10% when they receive ARV therapy during labor, and prophylactic ARV therapy is administered to their HIV‑exposed infant.
Define existing practices and identify performance gaps
Detailed review of cases where MTCT occurred was performed to identify performance gaps based on six main variables: (1) adequacy of prenatal care (2) HIV diagnoses of expectant mothers prior to delivery (3) appropriate use of ARV therapy before delivery (4) appropriate use of cesarean section for delivery (5) adequacy of zidovudine prophylaxis to newborn (6) HIV transmission rate.
In 2005–2006, pregnant women in Nevada were only screened for HIV if they were identified as “high risk” by their obstetricians. Only one hospital in Clark County had a well‑defined protocol for screening pregnant women who presented in labor with unknown HIV status. Only one center provided comprehensive care for HIV‑infected pregnant women in Clark County with a population of 1.9 million in 2006. SNHD maintains data on individuals with HIV/AIDS, but there were no systematic methods for the hospitals, obstetricians, and pediatricians to confirm the HIV status of pregnant women to allow for early intervention. No pediatric program was dedicated to the follow‑up of infants who had been perinatally exposed to HIV, and there was no defined communication between the SNHD, the obstetricians and pediatrician providing surveillance, or prenatal and pediatric care.
Design an intervention and define outcome measures
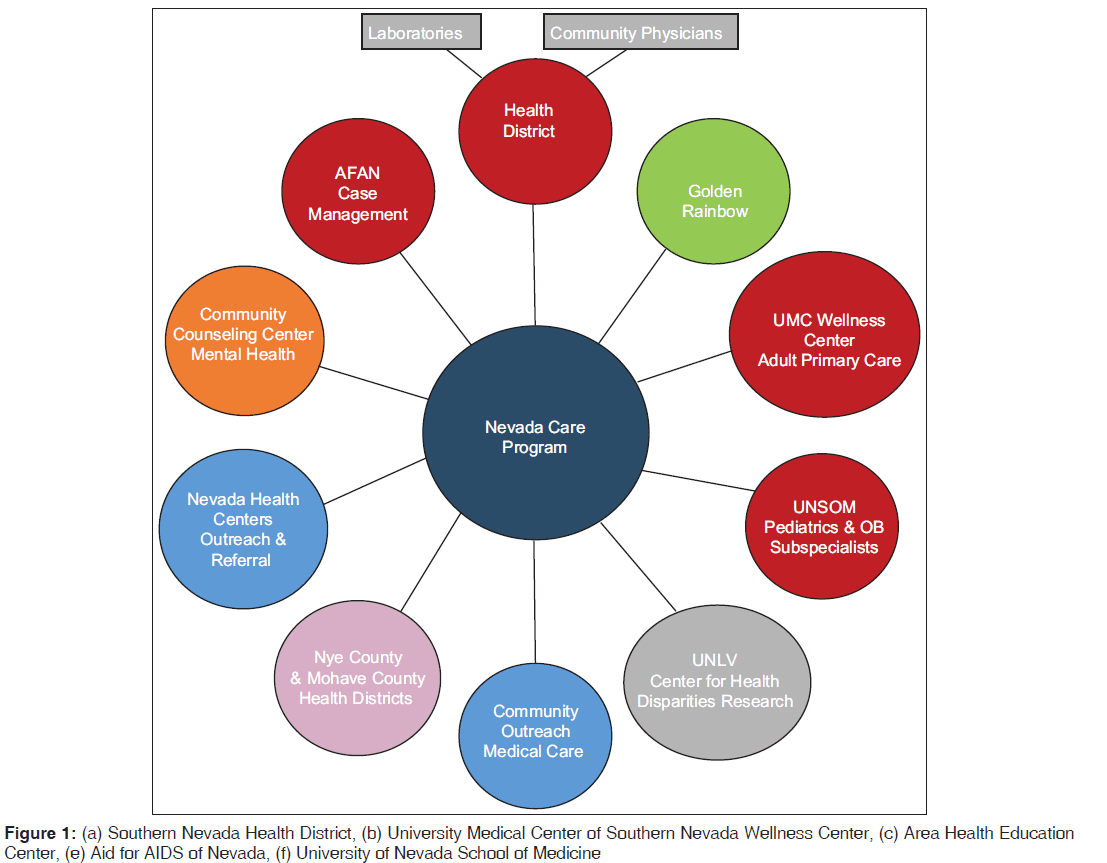
Information obtained from our review of performance gaps was used to design a program to address identified barriers. Five community organizations were invited to partner with the UNSOM in developing an intervention program that would integrate services provided by SNHD and community organizations with clinical services provided by the UNSOM Departments of Pediatrics and Obstetrics. Each agency was assigned specific roles [Figure 1]. A 7‑step integrated intervention for the care of HIV‑infected pregnant women and HIV‑exposed infants was developed [Table 1]. For the purpose of this study and in order for consistency in evaluating pre‑ and post‑intervention outcomes, certain terms were defined as follows: (a) adequate prenatal care was defined as cases where a pregnant woman with HIV had at least two prenatal visits prior to delivery; (b) HIV‑infected pregnant women were considered to have received appropriate ARV therapy during pregnancy if the combination ARV therapy prescribed was “preferred” in USPSTF’s recommendations for HIV treatment were instituted prior to labor; (c) appropriate use of cesarean section for delivery was defined as cesarean section delivery for a HIV‑infected pregnant woman with the most recent viral load prior to labor above 1000 copies/ml or for other medical reasons including previous cesarean section; (d) adequacy of zidovudine prophylaxis to newborn was defined as initiation of zidovudine within 12 h of birth and completion of prophylaxis for a 6 weeks following birth; (e) a child was defined to be HIV positive if he/she was < 18 months with detectable HIV pro‑viral particle by qualitative HIV DNA polymerase chain reaction on two separate specimens and HIV negative if he/she had two negative HIV test obtained at or after 1‑month.
| Positive HIV tests are reported to the Clark County Health Department from all laboratories and physician practices as mandated by state law |
| Health Department Surveillance team reaches out to contact patient, and if confirmed pregnant, brings it to the attention of the maternal‑child HIV team |
| Pregnant woman is assisted in enrolling into care at the wellness center under the care of an adult HIV specialist and an obstetrician. Patients are also assisted in identifying other care providers and obstetricians not within the county hospital system if they so desire |
| Pregnant women are scheduled to meet with pediatrician to discuss expected plan of care for their infant once he/she is delivered. Education is provided with regards to risk of transmission and available interventions to reduce risk of transmission |
| Social support is provided through the health department and AFAN including but not limited to transportation and housing as needed |
| All pregnant women presenting in labor at all hospitals in Las Vegas were assessed for documented HIV sero‑status. Rapid HIV testing is performed on all pregnant women with unknown HIV sero‑status unless patient declines |
| Patients are discussed during a monthly clinical meeting where barriers to care are assessed, identified and a specific plan was developed to eliminate or reduce barrier |
Table 1: Seven‑step approach to care of HIV‑infected pregnant women and HIV‑exposed infants
Evaluate system improvement
Six predefined outcome measure were used to evaluate system improvement after 6 years (2007–2012).
• adequacy of prenatal care
• HIV diagnoses of expectant mothers prior to delivery
• appropriate use of ARV therapy before delivery
• appropriate use of cesarean section for delivery
• adequacy of zidovudine prophylaxis to newborn
• HIV transmission rate.
Evaluate health outcomes and disseminate findings
Final HIV sero‑status of the infant using appropriate diagnostic test for exposed infants was used to evaluate and define health outcomes and health‑related quality of life. All descriptive and inferential statistics were calculated using IBM SPSS version 15.0.
Results
Overall
A review of the database for HIV infection maintained by the SNHD revealed that the final HIV status of all infants born between 2000 and 2004 were indeterminate due to “loss to follow‑up” that did not allow a final HIV status to be established. In 2005, there were 5406 persons living with HIV/AIDS in Clark County, 495 (9%) were women of childbearing age. Twenty‑six infants were born to women with HIV between September 2005 and June 2006. One hundred and five infants were born to women with HIV from 2007 to 2012. Demographic information is provided in Table 2. Of the HIV‑positive women, 69% had Medicaid, 5% were uninsured and 27% had private health insurance.
| Exposed infants | Sex | Race/ethnicity | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Year of birth | Number of births | Males | Females | African American | Hispanic | Caucasian | Native American | Pacific Islander/Asian | Other |
| Pre‑intervention | |||||||||
| 2005* | 5 | 2 | 3 | 2 | 2 | 0 | 0 | 0 | 1 |
| 2006** | 21 | 13 | 8 | 9 | 8 | 4 | 0 | 0 | 0 |
| Total | 26 | 15 | 11 | 11 | 10 | 4 | 0 | 0 | 1 |
| Post‑intervention | |||||||||
| 2007 | 20 | 10 | 10 | 11 | 4 | 4 | 0 | 0 | 1 |
| 2008 | 19 | 7 | 12 | 10 | 3 | 4 | 1 | 1 | 0 |
| 2009 | 22 | 10 | 12 | 10 | 8 | 2 | 0 | 0 | 2 |
| 2010 | 24 | 8 | 16 | 13 | 5 | 5 | 0 | 0 | 1 |
| 2011 | 10 | 6 | 4 | 7 | 1 | 1 | 0 | 0 | 1 |
| 2012 | 10 | 4 | 6 | 7 | 1 | 1 | 0 | 0 | 1 |
| Total | 105 | 45 | 60 | 58 | 22 | 17 | 1 | 1 | 6 |
Table 2: Demographic characteristics of mothers: Pre‑ and post intervention
Prior to 2007, only one hospital implemented a rapid HIV testing during labor for women presenting in labor with unknown HIV sero‑status. At the end of 2012, all ten local hospitals in Clark County with a labor and delivery unit had a protocol for rapid HIV testing for women presenting in labor with unknown HIV sero‑status.
Evaluate system improvement
We evaluated improvements in the six predefined outcome measure after 6 years.
Among the 26 HIV‑infected women who delivered prior to the implementation of the integrated program, 58% (15/26) had adequate prenatal care. Among women who delivered following the implementation of the integrated intervention, 85% (89/105) had adequate prenatal care. Preintervention, 46% (12/26) of HIV‑positive mothers were diagnosed prior to pregnancy, 35% (9/26) during pregnancy, 4% (1/26) during labor and 15% after delivery. Postintervention, 63% (66/105) of HIV‑positive mothers were diagnosed prior to pregnancy, 31% (33/105) during pregnancy, 5% (5/105) during labor and 1% (1/105) after delivery.
Lack of appropriate screening during pregnancy, labor and delivery led to missed opportunities to initiate ARV therapy to pregnant women. Of the 26 HIV‑positive women who delivered from September 2005 to June 2006, 62% (16/26) received appropriate ARV therapy during pregnancy, and 73% (19/26) received ARV therapy during labor. Postintervention, 81% (85/105) of the HIV‑positive women, received ARV therapy during pregnancy, and 86% (90/105) received ARV therapy during labor.
Preintervention, 62% (16/26) of HIV‑infected pregnant received appropriate delivery by cesarean section. Postintervention, cesarean sections were performed on 74% (78/105) of the HIV‑infected mother and all (100%) were judged to be medical appropriate. We made this determination by reviewing our cesarean section cases and found that the majority of cases were due to the history of previous cesarean and request by the pregnant women for repeat cesarean section. Cesarean sections were not related to persistent lack of viral suppression.
Only 69% (18/26) of the 26 infants born from September 2005 to June 2006 received adequate zidovudine prophylaxis defined as initiation of zidovudine within 12 h of birth and 54% (14/26) had documented completion of 6 weeks therapy with zidovudine. Postintervention, 87% (91/105) of HIV‑exposed infants, received zidovudine within 12 h of birth, and 87% (91/105) had documented completion of 6 weeks therapy with zidovudine.
Six infants were documented to have been infected with HIV among the 26 infants delivered during the preintervention period September 2005 through June 2006. No MTCT was documented among the 105 infants born postintervention from 2007 to 2012.
Discussion
The World Health Organization in its recent publication of PMTCT strategic vision 2010–2015 outlined that “priority will be given to strengthening linkages between PMTCT and HIV care and treatment services for women, their children, and other family members in order to support an effective continuum of care.”[22] Such an integrated approach between public health departments, primary care practices and hospitals, provides support to women who are known to be HIV‑infected or test positive for HIV during pregnancy and is also in line with the World Health Organization and the IOM’s recommendations.[22,23] The result from our program validates the point that MTCT of HIV can be eliminated when an integrated approach to the care of HIV‑infected women and exposed newborns is implemented.
Although women accounted for an estimated 8% of HIV/AIDS infected adults in 1985, that proportion had increased steadily to an estimated 25% of new infections in 2006, with a majority of infections occurring among women of childbearing age.[24] Studies evaluating missed opportunities to prevent perinatal HIV transmission in the United States conducted between 1996–2000 and 2005–2008 noted that the majority of HIV‑infected pregnant women had one or more missed opportunities to prevent perinatal HIV transmission.[25]
In response to the six cases of perinatal HIV‑infection in newborns in 2005–2006, we began the process of implementing the comprehensive HIV program in Clark County. To obtain buy in from the community hospitals, we formed the community advisory board for the elimination of pediatric HIV. The advisory board was comprised of staff representatives from pediatric and adult HIV clinics, nursing case managers from the county Health Department and hospital representatives from the 10 local hospitals that had a delivery unit. This committee met once a month and reviewed the national HIV perinatal guideline to produce a local version that detailed the management of women who present in labor with known and unknown HIV status and their infants. These hospital representatives, who were in most cases nurses and directors of their hospital delivery units, were critical to the success of our program. They acted as liaisons between the hospitals and the SNHD. They were the contact person to verify the HIV status of women presenting in labor through the county name‑based database. The privacy and confidentiality requirement was maintained through existing memorandum between the hospitals and the health department.
Once the local guidelines were approved by the hospitals, we embarked on a 6 months training session where in‑service trainings were conducted in all the hospitals. Each hospital had four training sessions organized in such a manner that it occurred during the morning and evening hand‑over session and included the nursing and laboratory staff. This allowed the team the opportunity to reach most of the nursing and laboratory staff including those on day and night shifts. The training curriculum included appropriate test requisitions, rapid HIV testing by the laboratory team, a protocol for the management of the HIV‑exposed infant including the appropriate blood specimen for testing.
The program team met once a month with the nursing case management team from the health department. Under an existing memorandum of understanding, we discussed each new HIV case documented in a pregnant woman. We also reviewed the care of existing pregnant women who were in care to identify barriers to care especially social issues that included but were not limited to transportation and housing during pregnancy. We discussed postpartum follow‑up and discharge of infants from the program to their regular pediatricians once HIV infection had been ruled out. A result of the work of the program team was mandatory HIV screening for all pregnant women, which was implemented in Nevada following the passage of Nevada Senate Bill 266. This bill was passed in 2007 and was instrumental for enhanced identification of HIV‑infected women who became pregnant.[26] The comprehensive nature of this intervention and the taskforce approach was instrumental to reducing the missed opportunities for PMTCT in our community.
After the integrated intervention, women who were identified early in their pregnancy had multiple opportunities to be brought into care. The integrated approach provided coordination and collaboration where prenatal care was provided by an obstetrician. In addition, they meet at least once with the pediatric infectious diseases physician during pregnancy to discuss factors that affected the risk of perinatal transmission and to develop a plan of care once the infant was delivered. Our report shows that such initial contact with a pediatrician led to increased compliance with follow‑up of the infant and compliance with postnatal zidovudine prophylaxis. Approximately 69% of our patient had some form of public sponsored insurance which presented an initial challenge to enrollment into prenatal care, but ultimately removed cost as a barrier to prenatal care attendance.
Our report shows that lack of prenatal screening for HIV during pregnancy and labor increased the risk that HIV‑infected women were not identified in time and opportunities for initiating zidovudine prophylaxis were missed. The lack of a coordinated program led to poor follow‑up of HIV‑exposed infants and adherence to zidovudine prophylaxis during the preintervention period which improved dramatically to 87% postintervention. We believe that early involvement of a pediatrician can tremendously improve follow‑up after delivery as relationship are established early, and a clear follow‑up plan is developed. This analysis showed that all cases of perinatal transmission in the preimplementation period of the integrated program were among minority women (25% Hispanics and 75% African American) who had limited or no prenatal care. This is consistent with recent results in the US that showed that during 2007–2009, 85% of diagnoses of perinatal HIV‑infection were in Blacks (63%) or Hispanics (22%).[27] Overall, while the proportion of women with HIV infection has risen in the US, the number of reported cases of perinatal transmission has declined from an estimated annual peak of 1650 infected infants in mid‑1990s to 162 infants in 2010.[27] Our finding of no cases of perinatal transmission diagnosed postimplementation is consistent with other studies that showed reductions in perinatal transmission with successful implementation of strategies aimed at identifying HIV‑infected pregnant women before or early in pregnancy, treating HIV‑infection in pregnant women with highly active ARV therapy, zidovudine prophylaxis during labor and delivery, and zidovudine prophylaxis to HIV‑exposed infants.[10]
Limitations
Our analysis has a number of limitations. First, it is a single site experience, and even though it included all deliveries in the county, our experience may be different from other part of the country. Second, care for HIV‑infected adults and children were concentrated in two major medical centers in our community, and it was easier to implement an integrated program. It may be more difficult to implement in communities without consolidated HIV care centers. Thirdly, successful passage of the Nevada Senate Bill mandating HIV screening of all pregnant women in our community could have made our educational and outreach interventions more successful by allowing for increased communication between obstetricians and pediatricians and greater collaboration among HIV service organization, hospitals and the health district.
Conclusion
Our study indicated that an integrated approach to the care of pregnant HIV‑infected women and their newborns can led to a reduction in missed opportunities for prevention and eventual eradication of perinatal HIV transmission by increasing the odds that the women and their newborns receive recommended interventions.
Ethical approvals
This project received ethical approval from the University of Nevada Institutional Review Board and the Institutional Review Board of the University Medical Center of Southern Nevada.
References
- The mode of delivery and the risk of vertical transmission of human immunodeficiency virus type 1 – A meta‑analysis of 15 prospective cohort studies. The International Perinatal HIV Group. N Engl J Med 1999;340:977‑87.
- de MartinoM, TovoPA, TozziAE, PezzottiP, GalliL, LivadiottiS, et al. HIV‑1 transmission through breast‑milk: Appraisal of riskaccording to duration of feeding. AIDS 1992;6:991‑7.
- Whitmore SK, Taylor AW, Espinoza L, Shouse RL, Lampe MA, Nesheim S. Correlates of mother‑to‑child transmission of HIV in the United States and Puerto Rico. Pediatrics 2012;129:e74‑81.
- Connor EM, Sperling RS, Gelber R, Kiselev P, Scott G, O’Sullivan MJ, et al. Reduction of maternal‑infant transmission of human immunodeficiency virus type 1 with zidovudine treatment. Pediatric AIDS Clinical Trials Group Protocol 076 Study Group. N Engl J Med 1994;331:1173‑80.
- Cooper ER, Charurat M, Mofenson L, Hanson IC, Pitt J, Diaz C, et al. Combination antiretroviral strategies for the treatment of pregnant HIV‑1‑infected women and prevention of perinatal HIV‑1 transmission. J Acquir Immune Defic Syndr 2002;29:484‑94.
- Lindegren ML, Byers RH Jr, Thomas P, Davis SF, Caldwell B, Rogers M, et al. Trends in perinatal transmission of HIV/AIDS in the United States. JAMA 1999;282:531‑8.
- Centers for Disease Control and Prevention (CDC).Achievements in public health. Reduction in perinatal transmission of HIV infection – United States, 1985‑2005. MMWR Morb Mortal Wkly Rep 2006;55:592‑7.
- Centers for Disease Control and Prevention. Reduction in perinatal transmission of human immunodeficiency virus ‑ United States, 1985‑2006. MMWR 2006;21:592‑7.
- Branson BM, Handsfield HH, Lampe MA, Janssen RS, Taylor AW, Lyss SB, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health‑care settings. MMWR Recomm Rep 2006;55:1‑17.
- Nesheim S, Taylor A, Lampe MA, Kilmarx PH, Fitz Harris L, Whitmore S, et al. A framework for elimination of perinatal transmission of HIV in the United States. Pediatrics 2012;130:738‑44.
- A Profile of Children Born to HIV Infected Mothers in Nevada: 1994‑2003. Bureau of Community Health and Bureau of Health Planning Statistics. Nevada State Health Division; October, 2005.
- Lampe MA. “Perinatal HIV Prevention: Successes and Challenges in the United States.” Division of HIV/AIDS Prevention; National Center for HIV, STD, and TB Prevention Centers for Disease Control and Prevention. World Aids Day Presentation, Las Vegas; December 01, 2006.
- CDC HIV/AIDS Surveillance Report, 2004. Vol. 16. Atlanta: US Department of Health and Human Services, CDC; 2005. p. 1‑46. Available from: http://www.cdc.gov/hiv/ topics/surveillance/resources/reports/2004report/pdf. [Last accessed on 2008 Sep 02].
- Ezeanolue EE, Schenauer C. Challenges to the elimination of mother‑to‑child transmission of HIV infection: Four case reports. AIDS Read 2007;17:33‑8.
- Wodi AP, Ezeanolue EE. Overcoming the barriers to successful elimination of perinatal HIV transmission. Infect Med 2007;24:304‑6.
- Veteran Affairs QUERI Six Step Process Model. Available from: http://www.rehab.research.va.gov/meet/queri/ six‑step‑process.pdf. [Last accessed on 2014 Oct 14].
- Nevada State Health Division ~ HIV/AIDS Surveillance Program. HIV/AIDS Fast Facts; 2006. Available from: http://www.health.nv.gov/docs/fastfacts2006 hivaids.pdf. [Last accessed on 2008 Sep 02].
- Institute of Medicine, Committee on Perinatal Transmission of HIV and Commission on Behavioural and Social Sciences and Education. Reducing the Odds: Preventing Perinatal Transmission of HIV in the United States. Washington, DC: National Academy Press; 1999.
- Public Health Service Task Force. Recommendations for Use of Antiretroviral Drugs in Pregnant HIV‑1‑Infected Women for Maternal Health and Interventions to Reduce Perinatal HIV‑1 Transmission in the United States ‑ Living Document.Available from: http://aidsinfo.nih.gov/contentfiles/ lvguidelines/perinatalgl.pdf. [Last accessed on 2014 Oct 14].
- Human immunodeficiency virus screening. Joint statement of the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists. Pediatrics 1999;104 (1 Pt 1):128.
- American College of Obstetrics and Gynecology. Prenatal and Perinatal Human Immunodeficiency Virus Testing: Expanded Recommendations. Available from: http:// www.acog.org/Resources%20And%20Publications/ Committee%20Opinions/Committee%20on%20Obstetric%20 Practice/Prenatal%20and%20Perinatal%20Human%20 Immunodeficiency%20Virus%20Testing%20 ‑ %20 Expanded%20Recommendations.aspx. [Last accessed on 2006 Sep 02].
- World Health Organization. PMTCT Strategic Vision 2010‑2015: Preventing Mother‑to‑Child Transmission of HIV to Reach the UNGASS and Millennium Development Goals. Available from: http://www.who.int/hiv/pub/mtct/ strategic_vision.pdf. [Last accessed 2014 Oct 14].
- Primary Care and Public Health: Exploring Integration to Improve Population Health. Institute of Medicine. Report Brief. Available from: http://www.iom.edu/ primarycarepublichealth. [Last accessed on 2013 Apr 08].
- Center for Disease Control and Prevention. HIV/AIDS and Women. Available from: http://www.cdc.gov/hiv/topics/ women/index.htm. [Last accessed on 2013 Apr 08].
- Peters V, Liu KL, Dominguez K, Frederick T, Melville S, Hsu HW, et al. Missed opportunities for perinatal HIV prevention among HIV‑exposed infants born 1996‑2000, pediatric spectrum of HIV disease cohort. Pediatrics 2003;111:1186‑91.
- Nevada Senate Bill 266. Available from: http://www. leg.state.nv.us/74th/FiscalNotes/3527.pdf. [Last accessed 2014 Oct 14].
- Center for Disease Control and prevention. HIV among Pregnant Women, Infants, and Children in the United States. Available from: http://www.cdc.gov/hiv/topics/perinatal/ index.htm. [Last accessed 2014 Oct 14].




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.