Yoga for High‑Risk Pregnancy: A Randomized Controlled Trial
- *Corresponding Author:
- Dr. Tikhe Sham Ganpat
S-VYASA University, Bangalore, India.
E-mail: rudranath29@gmail.com
Abstract
Background: Improvements in technology have increased the chances of survival for the micro‑premature infant and the very low birth‑weight infant but have significantly increased the financial burden of health care organizations. This economic burden has a significant impact on third‑party payers and on society in general. Aim: The study was designed to assess yoga therapy (YT) module on maternal stress level in high risk pregnancy. Subjects and Methods: In the present study, sixty‑eight pregnant women (38 in the control group with standard antenatal care and 30 in the YT group) with 27.2 (5.2) years of mean age recruited from the outpatient services of medical college and hospital in Bangalore, South India, were participated. The study was a single‑blind randomized controlled clinical trial. Perceived stress scale (PSS) was measured during the 12th, 20th, and 28th weeks of pregnancy. SPSS version 16.0 (Chicago, IL, USA) was used for all data analysis. When the data were found to be normally distributed,the RMANOVA were used to assess the PSS scores between the yoga and control groups. Significant values were set at P < 0.05. Results: There was a significant difference in the PSS level of the YT group with significantly reduced scores at the second follow‑up (28th week of pregnancy) compared to the control group (P = 0.02). Women who took part in the YT module reported significantly fewer pregnancy discomforts decrease in PSS (P = 0.02) than the control group where the stress level was increased (RMANOVA test using SPSS‑16). Conclusion: The present study suggests that the YT module can decrease the stress level during high‑risk pregnancy complications. Thus, practicing YT during high‑risk pregnancy is not only a cost‑effective option but also a feasible and safe option. Additional well‑designed studies are needed before a strong recommendation can be made.
Keywords
High-risk pregnancy, Maternal stress level, Yoga therapy module
Introduction
There are no clearly identified criteria to distinguish between a “high”- or “low”-risk pregnancy; however, pregnancies in which the maternal and/or fetal condition pose a threat to life of the mother or fetus are considered as “high risk.”[1] Maternal conditions most commonly associated with adverse prenatal outcomes include conditions such as diabetes (chronic and gestational), hypertensive disorders (chronic hypertension, and preeclampsia) and cardiac, renal, autoimmune, and thrombophiliac disorders.[2-4] Fetal conditions associated with high-risk pregnancy (HRP) include fetal growth restriction, and placental insufficiency.[5-7] Sound theoretical knowledge about various complicated conditions and diseases that may interfere with childbearing is essential in the care of pregnant women at high risk. Pregnant women at risk want to be treated as normal and help her get through pregnancy and birth with as little sickness and complication as possible[8] Improvements in technology have increased the chances of survival for the micro-premature infant and the very low birth-weight infant but have significantly increased the financial burden of health care organizations. This economic burden has a significant impact on third-party payers and on society in general. Of the annual U.S. 10.2 billion dollars spent on newborn care alone, 57% is disproportionately consumed by the 10% of infants who are born preterm.[9] Therefore, it is important to take into consideration the economical and social dimension of woman when directing treatment during pregnancy.
Studies have shown that fetuses of exercising women may tolerate labor better than those of nonexercisers.[10] It has been suggested that regular physical activities may protect against preeclampsia by intervening at three key stages in the disease process: (1) enhanced placental growth and vascularity (protection against abnormal placental development), (2) reduction of oxidative stress, and (3) reversal of endothelial dysfunction.[11] Yoga, an ancient science of holistic living has been used for centuries in stress reduction and health promotion[12] and its positive effects have been demonstrated even in women with HRP complications.[13] An integrated approach to yoga during pregnancy improved birth weight, decreases preterm labor, and decreases intra uterine growth retardation (IUGR) either in isolation or associated with pregnancy-induced hypertension, with no increased complications.[14]
With these promising benefits of yoga, we could hypothesize that yoga therapy (YT) module may play a vital role in prevention of HRP. But, there was insufficient evidence for the role of the YT module in a randomized control trial for prevention of HRP. Hence, the present study was designed to assess the efficacy of the YT module in reduction of maternal stress in HRP, with the hypothesis that it is possible to select safe stress reducing practices.
Subjects and Methods
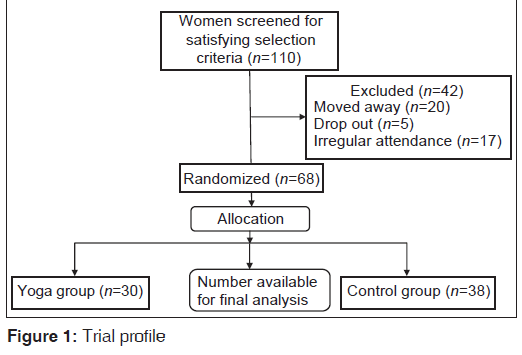
Patients with a diagnosis of HRP, who were on regular follow-up and willing to give consent for the study, were recruited from the outpatient services of the Medical College and Hospital in Bangalore, South India. A total of 68 patients were included in the study with their age ranging from 19 to 31 [mean (SD), 27.4 (5.1)] years. The reasons for exclusion of 42 women from the study were as follows: moved away (n = 20), drop out (n = 5) and irregular attendance (n = 17). There were 18 (8 yoga, 10 control) women with bad obstetric history, 14 (6 yoga, 8 control) with age factor, 14 (6 yoga, 8 control) with genetics, 13 (6 yoga, 7 control) with obesity, 8 (4 yoga, 4 control) with multiple pregnancy, and 1 (control) with diabetes. Signed informed consent was obtained from all subjects before randomization and the project had received clearance from the ethical committee of University in Bangalore, South India prior to recruitment of the subjects. Furthermore, the project was approved by the Institutional Ethical Review Board and the registration number was IERB/1/861/08. The project was also registered with Clinical Trial Registration of India (CTRI) with registration number as CTRI/2011/10/002096. Patients with a diagnosis of HRP were selected using following criteria:
Inclusion criteria
Pregnant women with (1) hypertension at the time of recruitment/prior to this pregnancy, (2) diabetes at the time of recruitment/prior to this pregnancy, (3) past history of pregnancy complications such as pregnancy-induced hypertension (PIH), gestational diabetes mellitus (GDM), pre-eclampsia (PE) or eclampsia (E), intrauterine growth restriction (IUGR), placental abruption (PA), and fetal death (FD), (4) multiple pregnancies, (5) extremes of age, i.e., <20 or > 35 years, (6) BMI > 30, (7) family history (sister, mother, and/or grandmother) of pregnancy complications (PIH, GDM, PE or E, IUGR, PA, FD).
Exclusion criteria
Pregnant women with (1) major medical (cardiac, renal or neurological diseases) or mental illnesses (psychosis, neurosis, addictions, etc.) or with any structural abnormality of reproductive system and (2) normal pregnancy.
The present study was a single-blind randomized controlled clinical trial. Using computer-generated random numbers, 68 patients were allocated to two treatment groups: Yoga (n = 30), control (n = 38) at their 12th week of pregnancy (end of the first trimester). The power analysis (alpha = 0.01, power = 0.8, effect size = 0.81) had yielded 27 subjects per group.
The YT module used in this study was selected carefully by the investigators based on previous studies.[13,15] This module was a holistic approach to well-being at physical, mental, emotional, intellectual, and spiritual levels and was designed to reduce chronic psychological stress experienced during HRP. The practices for the control group involved standard simple prenatal stretching exercises approved by the Society of Obstetricians and Gynecologists of Canada (SOGC) Clinical Practice Obstetrics Committee, the Executive and Council of SOGC, and the Board of Directors of the Canadian Society for Exercise Physiology.[16]
The outcome measure was the perceived stress scale (PSS) scores. The PSS is a widely used valid psychological instrument for measuring perception of stress in the Indian population with a Cronbach’s α for reliability of 0.84.[17,18] This questionnaire consists of 10 questions about experiencing stress during the previous month and coping with the stress, and has a 5-point scoring system from 0 to 4 with reverse scoring for 4 positive items (the 4th, 5th, 7th, and 8th questions).[19] The final score is a sum of the scores for all 10 items. The PSS questionnaire was administered at the baseline, i.e., 12th week of pregnancy, 20th week of pregnancy (1st follow-up), and 28th week of pregnancy (2nd follow-up).
Randomization was carried out using a computer-generated random number table and all baseline data were collected prior to the starting of prenatal treatment (YT module). The fact that there was no baseline differences in the yoga and control groups helped to compare the data at follow-up without adjusting for the means at baseline. This study was a single-blind, randomized controlled clinical trial where only the patients, the medical staff, and the yoga instructor knew the treatment group. The people involved in the assessments were blind to the group treatment status.
Statistical software SPSS version 16.0 (Chicago IL.USA) was used for all data analysis. When the data were found to be normally distributed by a Kolmogorov–Smirnov test (P > 0.05), the RMANOVA were used to assess the PSS scores between the yoga and control groups.
Results
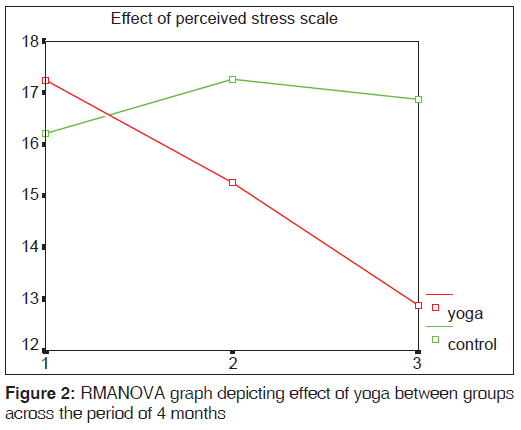
The trial profile shows the selections process of the subjects for the study [Figure 1]. The socio-demographic data showed that there was no significant difference in any of the demographic or clinical variables in both the yoga and control groups [Table 1]. The independent sample t-test showed that there was no significant difference in the PSS scores between the yoga and control groups at baseline. This showed that the sample in both the groups were comparable at the same PSS score level at the start of the study. There was also no significant difference in the PSS scores between the groups at the first follow-up (20th week of pregnancy). However, a significant difference in the PSS scores (P = 0.02) of the yoga group with reduced scores at the second follow-up (28th week of pregnancy) compared to the control group was observed [Table 2]. Since PSS scores were collected at three time periods, i.e., baseline (12th week of pregnancy), first follow-up (20th week of pregnancy), and second follow-up (28th week of pregnancy) across two groups (yoga and control), the RMANOVA was conducted to assess PSS scores across the groups over the period of time. The results of the RMANOVA showed that there was a significant decrease (P = 0.02) in the PSS scores of the yoga group compared to the control group [Figure 2].
| Variable | Yoga (n=30) Mean (SD) | Control (n=38) Mean (SD) | P value* |
|---|---|---|---|
| Age | 27.7 (5.1) | 27.2 (5.2) | 0.69 |
| Income (in thousands) | 37.3 (11.3) | 36.5 (8.5) | 0.60 |
| Religion | |||
| Hindu | 25 (83.3) | 29 (76.3) | |
| Muslim | 0 | 4 (10.5) | 0.18 |
| Christian | 5 (16.7 | 5 (13.2) | |
| Complications in | |||
| pregnancy | |||
| Age factor | 6 (20.0) | 8 (21.1) | |
| Bad history | 8 (26.7) | 10 (26.3) | |
| Diabetes | 0 | 1 (2.6) | 0.96 |
| Genetics | 6 (20.0) | 8 (21.1) | |
| Multiple pregnancy | 4 (13.3) | 4 (10.5) | |
| Obesity | 6 (20.0) | 7 (18.4) |
*Independent samples t-test, SD: Standard deivation
Table 1: Demographic dat
| Variable | Yoga (n=30) Mean (SD) | Control (n=38) Mean (SD) | F value | P value |
|---|---|---|---|---|
| PSS baseline | 17.00 (6.03) | 16.00 (5.97) | F1=2.47 | 0.09 |
| PSS first follow-up | 15.28 (5.64) | 17.11 (6.17) | F2=583.39 | <0.001** |
| PSS second follow-up | 12.92 (6.09) | 16.88 (6.03) | F3=4.29 | 0.02* |
*P<0.05; **P<0.01; RMANOVA test, F1: Time effect, F2: Occasion effect, F3: Interaction effect, PSS: Perceived stress scale, SD: Standard deivation
Table 2: Perceived stress scale scores at baseline, first and second follow-up
Discussion
Many women would like to avoid pharmacological or invasive methods of pain management in labor and this may contribute toward the popularity of complementary methods of pain management. In this connection, it has been reported that relaxation and yoga may have a role with reducing pain, increasing satisfaction with pain relief, and reducing the rate of assisted vaginal delivery.[20] Previous study on yoga showed that yoga is a noninvasive, economical, and easy-to-learn solution to improve the quality of life of pregnant women, improve their abilities to perform their social roles, and potentially prevent adverse obstetrics outcomes. Pregnancy is a very special time in women’s life and yoga can give her the opportunity and tools to enjoy this miraculous period to the fullest.[15] It was demonstrated that meditation, breathing, and relaxation techniques which are the essential components of yoga have a direct and positive impact on the activities of the autonomic nervous system in a pregnant women.[14,21] The present study is consistent with these findings, indicating that systematic and safe adoption of the YT module can be effective in reducing the stress levels in HRP. Although, the present study was mainly focused on the prevention of HRP complications (we were forced to recruit very limited number of subjects in each high-risk category), it would be interesting and extremely useful to find out what would be the long-term benefits of the YT module on the mother and the child in pregnancies at high risk. The enhanced oxygenation in maternal blood, better circulation to and from placenta, and reduced maternal stress are certain to have long-term positive impacts on the health of the mother and the child.
Conclusion
The present study suggests that the YT module can decrease the stress level during HRP complications. Thus, practicing the YT module during HRP complications is not just a noninvasive and economical option but also a feasible and safe option. Additional well-designed studies are needed before a strong recommendation can be made.
Acknowledgement
This project was funded by Central Council of Research on Yoga and Naturopathy (CCRYN), Department of AYUSH, Government of India. We thank CCRYN, SJMC and H and S-VYASA University for supporting the project.
Source of Support
This project was funded by Central council of Research on yoga and Naturopathy (CCRYN).
Conflict of Interest
None declared.
References
- Alfirevic Z, Stampalija T, Gyte GM. Fetal and umbilical Doppler ultrasound in high-risk pregnancies. Cochrane Database Syst Rev 2010;(1):CD007529.
- Alfirevic Z, Roberts D, Martlew V. How strong is the association between maternal thrombophilia and adverse pregnancy outcome? A systematic review. Eur J Obstet Gynecol Reprod Biol 2002;101:6-14.
- Roos-Hesselink JW, Duvekot JJ, Thorne SA. Pregnancy in high risk cardiac conditions. Heart 2009;95:680-6.
- Westergaard HB, Langhoff-Roos J, Lingman G, Marsál K, Kreiner S. A critical appraisal of the use of umbilical artery Doppler ultrasound in high-risk pregnancies: Use of meta-analyses in evidence-based obstetrics. Ultrasound Obstet Gynecol 2001;17:466-76.
- Ashworth A. Effects of intrauterine growth retardation on mortality and morbidity in infants and young children. Eur J Clin Nutr 1998;52.
- Bernstein IM, Horbar JD, Badger GJ, Ohlsson A, Golan A. Morbidity and mortality among very-low-birth-weight neonates with intrauterine growth restriction. The Vermont Oxford Network. Am J Obstet Gynecol 2000;182:198-206.
- Miskovic B, Vasilj O, Stanojevic M, Ivankovi? D, Kerner M,Tikvica A. The comparison of fetal behavior in high risk and normal pregnancies assessed by four dimensional ultrasound. J Matern Fetal Neonatal Med 2010;23:1461-7.
- Berg M, Dahlberg K. Swedish midwives’ care of women who are at high obstetric risk or who have obstetric complications. Midwifery 2001;17:259-66.
- Hawkins MR. The impact of a high-risk disease management program on perinatal outcomes in a managed care organization. Case Manager 2005;16:59-63.
- Paisley TS, Joy EA, Price RJ Jr. Exercise during pregnancy: A practical approach. Curr Sports Med Rep 2003;2:325-30.
- Weissgerber TL, Wolfe LA, Davies GA. The role of regular physical activity in preeclampsia prevention. Med Sci Sports Exerc 2004;36:2024-31.
- Collins C. Yoga: Intuition, preventive medicine, and treatment. J Obstet Gynecol Neonatal Nurs 1998;27:563-8.
- Satyapriya M, Nagendra HR, Nagarathna R, Padmalatha V. Effect of integrated Yoga on stress and heart rate variability in pregnant women. Int J Gynaecol Obstet 2009;104:218-22.
- Narendran S, Nagarathna R, Narendran V, Gunasheela S, Nagendra HR. Efficacy of Yoga on pregnancy outcome. J Altern Complement Med 2005;11:237-44.
- Rakhshani A, Maharana S, Raghuram N, Nagendra HR, Venkatram P. Effects of integrated Yoga on quality of life and interpersonal relationship of pregnant women. Qual Life Res 2010;19:1447-55.
- Davies GA, Wolfe LA, Mottola MF, MacKinnon C, Arsenault MY, Bartellas E, et al. Exercise in pregnancy and the postpartum period. J Obstet Gynaecol Can 2003;25:516-29.
- Hewitt PL, Flett GL, Mosher SW. The Perceived Stress Scale: Factor structure and relation to depression symptoms in a psychiatric sample. J Psychopathol Behav Assess 1993;14:247-57.
- Chattha R, Nagarathna R, Padmalatha V, Nagendra HR. Effect of Yoga on cognitive functions in climacteric syndrome: A randomised control study. BJOG 2008;115:991-1000.
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1983;24:385-96.
- Smith CA, Levett KM, Collins CT, Crowther CA. Relaxation techniques for pain management in labour. Cochrane Database Syst Rev 2011;12.
- Kim HH, Nava-Ocampo AA, Kim SK, Kim SH, Kim YJ, Han JY, et al. Is prenatal childbirth preparation effective in decreasing adverse maternal and neonatal response to labor? A nested case-control study. Acta Biomed 2008;79:18-22.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.