A Survey on Selective Immunoglobulin A Deficiency Among Asthmatic Adults with Variable Total Immunoglobulin E levels in Tehran: An Office-Base Study
Citation: Agin K. A Survey on Selective Immunoglobulin A Deficiency Among Asthmatic Adults with Variable Total Immunoglobulin E levels in Tehran; An Office-Base Study. Ann Med Health Sci Res. 2018; 8: 118-121
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Selective IgA deficiency (SIgAD) is one of the most common primary antibody immunodeficiency diseases. The prevalence in Asia is lower than other areas. Asthma and allergic diseases are common among the SIgAD population. The aim of this study was to evaluate the prevalence of SIgAD among the adult asthmatic patients with variable immunoglobulin E (IgE) levels in serum. Patients and methods: 507 asthmatic patients of various age and sex who sequentially enrolled in the outpatient respiratory clinic were selected. Asthma diagnosis was based on the pulmonologist’s diagnostic and ATS criteria. IgA and total IgE levels in serum were measured according to manufacturer’s recommended kits. Results: 64 (13%) subjects detected as SIgAD. Mean age recorded 34.5 ± 13.9 SD years. The patient included 57% male and 43% female, respectively. Allergic asthma recorded 40% (205) of the study population. Conclusion: The SIgAD was remarkably found among Iranian adults with asthma. However, its frequency was lower in allergic asthma in comparison to the non-allergic subset. Additionally, the number of SIgAD subjects declined with increasing age. Detection of SIgAD among the asthmatic population may be effective in reducing complications.
Keywords
IgA deficiency; Selective IgA deficiency; Total IgE level; Allergy; Asthma; Adults Iranian
Introduction
Secretion of immunoglobulins A (IgA) is necessary for the defense mechanism of mucosal surfaces against infections and plays a significant role in the cleaning of foreign antigens. Individuals who are most frequented Selective Immunoglobulin A Deficiency (SIgAD), have been clinically healthy and who have had mild symptoms usually have been remained permanent in the adult population for their lifetime.
SIgAD is a universal primary immunodeficiency disease. [1] Its prevalence in Caucasians is up to (1:700). [2] While it is lower among Asia’s population. In Iran, it is up to (7.5%) [3] among adults. Prevalence distribution of SIgAD is different among social groups which suggest a genetic base for such disorder.[4]
The SIgAD subjects can be clinically associated with atopy, [5] allergic diseases, [6] asthma, [7] different autoimmune diseases and sinopulmonary infections. Its deficiency may lead to chronic inflammation of the airway in Chronic Obstructive Pulmonary Disease, [8] (COPD) and have a significant role in eosinophilic activation in asthma disease. [9] Moreover, it may be progressive to the most common variable immunodeficiency disease and lead to increased production of immunoglobulin E (IgE) in serum. [10]
Asthma is one of the most common diseases in the world that can be triggered with SIgAD, [11] with an estimated 300 million affected people [12] worldwide. Asthmatic patient is more prone to the risk of infections. It may be due to impaired innate and adaptive immune system that predisposes individuals to microbial infections or may be related to the presence of one type of primary immune deficiency such as; SIgAD. [13] Likewise, asthmatic patients are susceptible to the hypogammaglobinemia [14] caused by application of corticosteroids.
The objective of the study was to assess the status of SIgAD prevalence among the adult asthmatic patients with variable immunoglobulin E levels.
Patients and Methods
This study was cross-sectional and conducted in Shahid Beheshti University of Medical Sciences (SBMUS), Tehran- Iran. The study was designed based on the outpatient clinic’s asthmatic patients. Before starting at the study a consent form was received from all volunteers. Subjects sequentially enrolled and serum IgA and total IgE levels were initially evaluated. The entrance criteria consisted of asthmatic, adults of all age and both sexes with a recurrence of sinopulmonary infections and allergic symptoms in their medical history.
Asthma was defined based on an instruction of the American Thoracic Society (ATS) [15] and physician-diagnosed asthma. Accepted airway reversibility response to bronchodilator was improved up to 12% of FEV1 baseline or 200 ml of FEV1. The SIgAD was defined based on the following criteria; IgA level less than 70 mg /dl, normal IgM and IgG levels and age of diagnosis up to 14 years. The IgA was assayed in serum by an Immunoturbidimetry method with Biosystem kit (made in France) and Hitachi device measuring system. The total IgE (TIgE) also was measured by Elisa method of Pishtaz Co (Iran). The cutoff point which identifies allergy state was up to 200 Iu/ml.
The exclusion criteria were as based on the medical history, the SIgAD, malignancy, systemic diseases (losing protein enteropathy), infections (AIDS), consumption of immunosuppressant drugs, high –dose of corticosteroid, and known genetic diseases. [16]
The data included in the study were obtained using statistical program SPSS; version 22. The frequency and the mean of data were presented with percentage and mean ± SD. The normality was not detected by Kolmogorov-Smirnov test (Page, pIgA and PIgE= <0.001). Comparison of means was performed by nonparametric test; Kruskal-Wallis Test, Mann-Whitney Test, and Chi-Square Tests. The statistical significant value was set at P<0.05 throughout the study.
Results
A total of 507 subjects participated in the study. Characteristics of the sample population were defined based on the mean age of 34.5 ± 13.9 SD years. (Range 16-74, Median age 33 and Mode 16) The frequency of age was divided into several groups of classes as following: I (16-24) 31%, II (25-34) 23%, III (35- 44) 23%, IV (45-54) 15% and V (>55) 8% . All of asthmatic patients sample population included 57% male and 43% female. The study shows that the distribution of genders was approximately equal in all decades, but its frequency gradually decreases between 20s to 50s.
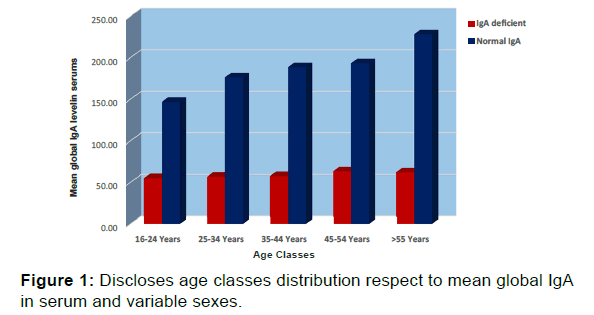
Figure 1 shows the distribution of age classes to mean global IgA in serum and among different sexes. Global of SIgAD frequency was 13% in asthmatic subjects. The frequency of SIgAD distribution was 33 (52%) in females and 31 (48%) in males. The mean of global IgA levels in the serum of asthmatic patients was 162.6 ± 81.5 mg/dl. The Minimum and the maximum values were 10 and 430 mg/dl, respectively, (with median 150mg/dl and Mode 100). Table 1 shows the characteristic of SIgAD and normal range IgA subsets. The frequency distribution of SIgAD was 29 within allergic asthma (6% sample study and 14% class) and 35 Non-allergic subsets (7% sample and 12% class). There were no significant differences between global serum IgA and TIgE levels in sample study (P=0.3).
| Subsets of asthmatic patients | Sex Male/Female |
Age Mean ± SD Year |
Serum IgE Mean ± SD Iu/ml |
Serum IgA Mean ± SD mg/dl |
Total number % |
|---|---|---|---|---|---|
| IgA deficient subclass | 31/33 | 30.8 ± 12.3 | 222.8 ± 240.9 | 57.3 ± 12.2 | 64 (13%) |
| Normal serum IgA | 259/184 | 35 ± 14 | 259.8 ± 247.4 | 178 ± 0.78 | 443 (87%) |
Table 1: Reveals statistical characteristics of Selective IgAD and normal IgA subsets.
The highest values of the SIgAD subjects were obtained in the 20s and 50s, respectively. Despite a difference in age and sex, the same frequency pattern was detected about global IgA level. A comparison of means was performed between serum TIgE, global IgA, and age with sex groups. Significant differences were detected between sex variable with serum TIgE, and age of study population (PIgE=0.03 and pAge=0.01). The frequency of SIgAD decreased along with increasing the age classes of asthmatic patients (older age).
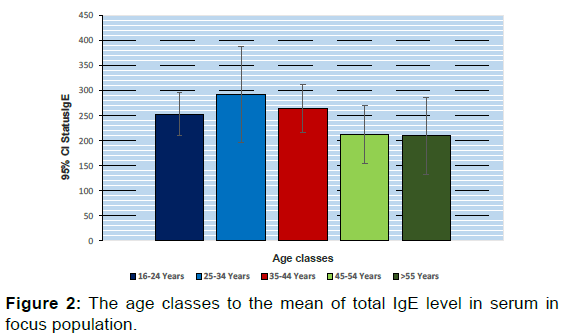
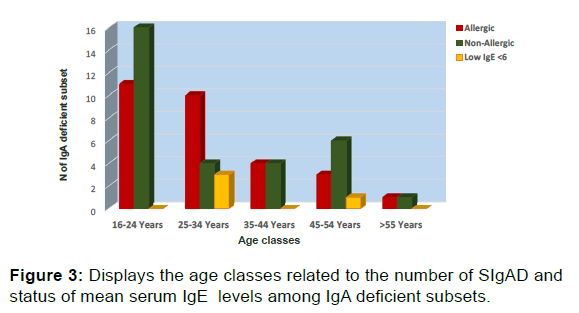
Figure 2 represents the relation between the age classes and the mean of TIgE level in serum, in sample study. In the population study, the mean of TIgE was 255, 02 ± 335.89 Iu/ml, (with median 137 and Mode 500). 40% (205) of sample study were allergic asthma. Allergic condition recorded more in 52% of the males. Moreover, the number of allergic individuals associated with raising the age decreased. Figure 3 displays the age classes related to the number of SIgAD and status of mean serum TIgE Low serum TIgE was detected in the sample study (1.8%). The SIgAD was more prevalent in recent finding 4 (6%). levels.
Discussion
IgA is the most abundant antibody isotype produced by the body secretions. Its functions have not been clearly understood by the immune system. IgA has two subclasses; monomeric IgA1 in serum and dimeric IgA2 in mucosal secretions. IgA deficiency (IgAD) is a result of a mutation in B-cells types [17] which are able to neutralize the intracellular bacterial pathogen (virus), bind to antigen at lamina propria by immune complex, prevent of the bacterial colonization by inhibition of adhesion mechanism, diminish inflammatory responses, [18] prevent the release of inflammatory cytokine (TNF-6, IL6) [19] and induced IL10 expression. [20]
85-90% of SIgAD are asymptomatic. It may be associated with a number of diseases and conditions such as; recurrent sinopulmonary infections, autoimmunity diseases, [21,22] allergic disorders 8 [23] and tumors (1.5%). [24] The prevalence of IgAD has been reported to be about 7.5% in Iranian population 3, in Caucasian 1:700 and is the lowest in Asian countries. [25] The only report that did not support the latter finding was related to Saudi Arabia that was reported in 1998 (45%). [26]
Asthma is a global disease that its prevalence progressively increases by 50% every ten years, particularly in developing countries. The frequency of allergy is following asthma burden. [27] Additionally, the allergic frequency was reported up to 40% worldwide. Similarly, the allergic asthma frequency was 40% [28] in our sample study as well. In the sample study, the numbers of allergic condition decreased with increasing age but the mean of TIgE levels was higher in other age classes. Allergic disorders have a higher frequency in younger people compared to older age. [29] This finding correlates with the number of allergic individuals and distribution in different age classes. The aging process is associated with markedly remodeled immune system both adaptive and innate, which is called immunosenescence. This leads to changes that result in increased susceptibility to chronic inflammation, enhanced Th2 and allergic inflammation. However, the genetic, genetic-environmental interactions and external risk factors are play role in development of allergic reactions among elderly. [30,31]
The increased TIgE in our study is especially debated among older- age classes. The earlier cohort study disclosed the inverse ratio between TIgE and aging. [32] Tow issues can be suggested as follow. Highly immunoglobulin E levels may not be associated with age-related changes, and a few of studies have been supported it. [33,34] Alternatively, the findings from our research may reflect the effects of external causal factors as environmental conditions on this asthmatic community. [35]
The allergen exposure is not the only mechanism of IgE production through mast cell activation. The humoral immune responses can reactivate the allergic responses by IgG, [36] raised IgG4 [37] and low-level secretory IgA antibodies. [38] In addition, IgAD individuals are more prone to atopic diseases.[39] Our endpoint results indicated that SIgAD consisted of 6% of the global study asthma population and 14% of the allergic asthmatic subset. It is an improvement with consideration of allergy prevalence within the primary IgAD.
Low–level IgE Patients are susceptible to more frequency presentation of autoimmune disease, multiple immunoglobulin deficiencies, and non-allergic airway bronchial hyper reactivity. [40] We found an undetectable level of TIgE among asthmatic samples (1.8%), in which, four subjects were SIgAD. The prevalence of IgE hypogammaglobinemia was reported in association with SIAD between 6, 4–32%. [41] The result of our study corroborated the recent investigations.
The IgA level in males was higher than females in normal condition. [42] It may be caused by gene control and environmental effects. [43] Sex differences distribution of SIgAD was higher in men than women. [44,45] The earlier finding was not in agreement with our results in the current study. However, the IgA level increased with increasing age. It was an improvement in our output and the number of SIgAD declined with increasing age classes.
Conclusion
In conclusion, the endpoint of the study relevantly represented the presence of SIgAD in the asthmatic population. SIgAD had more frequency in younger age class than older age. However, in the females, its frequency was lower in the allergic asthmatic subset with respect to the non-allergic subset and the number of SIgAD subjects declined with increasing age classes. The detection of SIgAD among the asthmatic population may be effective in reducing comorbid complications.
Acknowledgements
The author expressed his gratitude to all asthmatic patients who have supported us by providing personal and crucial information on this research.
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- Klemola T. Deficiency of immunoglobulin A. Ann Clin Res. 1987; 19: 248-257.
- Saghafi S, Pourpak Z, Aghamohammadi A, Pourfathollah AA, Samadian A, Farghadan M, et al. Selective immunoglobulin A deficiency in Iranian blood donors: Prevalence, laboratory and clinical findings. Iran J Allergy Asthma Immunol. 2008; 7: 157-162.
- Aghamohammadi A, Mohammadinejad P, Abolhassani H, Mirminachi B, Movahedi M, Gharagozlou M, et al. Primary immunodeficiency disorders in Iran: update and new insights from the third report of the national registry. J Clin Immunol. 2014; 34: 478-490.
- Hammarström L, Smith CIE. Genetic approach to common variable immunodeficiency and IgA deficiency. In: Ochs H, Smith CIE, Puck J, eds. Primary immunodeficiency diseases, a molecular and genetic approach. Oxford: Oxford University Press, 1999: 250-262.
- Santaella ML, Peredo R, Disdier OM. IgA deficiency: Clinical correlates with IgG subclass and mannan-binding lectin deficiencies. P R Health Sci J. 2005; 24: 107-110.
- Özcan C, Metin A, Erkoçoglu M, Kocabas CN. Bronchial hyperreactivity in children with antibody deficiencies. Allergol Immunopathol (Madr). 2015; 43: 57-61.
- Özcan C, Metin A, Erkoçoglu M, Kocabas CN. Allergic diseases in children with primary immunodeficiencies. Turk J Pediatr. 2014; 56: 41-47.
- Pilette C, Durham SR, Vaerman JP, Sibille Y. Mucosal immunity in asthma and chronic obstructive pulmonary disease: a role for immunoglobulin A?. Proc Am Thorac Soc. 2004; 1: 125-135.
- Aghamohammadi A, Mohammadi J, Parvaneh N, Rezaei N, Moin M, Espanol T, et al. Progression of selective IgA deficiency to common variable immunodeficiency. Int Arch Allergy Immunol. 2008; 147: 87-92.
- Michel FB, Guendon R, Guerrero AJ. Serum IgE in patients suffering from IgA deficiency with or without atopy. Nouv Presse Med. 1976; 5: 1811-1814.
- Papadopoulou A, Mermiri D, Taousani S, Triga M, Nicolaidou P, Priftis KN. Bronchial hyper-responsiveness in selective IgA deficiency. Pediatr Allergy Immunol. 2005; 16: 495-500.
- Braman SS. The global burden of asthma. Chest. 2006; 130: 4S-12S.
- Urm SH, Yun HD, Fenta YA, Yoo KH, Abraham RS, Hagan J, et al. Asthma and risk of selective IgA deficiency or common variable immunodeficiency: a population-based case-control study. Mayo Clin Proc. 2013; 88: 813-821.
- Hamilos DL, Young RM, Peter JB, Agopian MS, Iklé DN, Barka N. Hypogammaglobulinemia in asthmatic patients. Ann Allergy. 1992; 68: 472-481.
- Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005; 26: 948-968.
- Yel L. Selective IgA deficiency. J Clin Immunol. 2010; 30: 10-16.
- Pasquier B, Launay P, Kanamaru Y, Moura IC, Pfirsch S, Ruffié C, et al. Identification of FcalphaRI as an inhibitory receptor that controls inflammation: Dual role of FcRgamma ITAM. Immunity. 2005; 22: 31-42.
- Olas K, Butterweck H, Teschner W, Schwarz HP, Reipert B. Immunomodulatory properties of human serum immunoglobulin A: anti-inflammatory and pro-inflammatory activities in human monocytes and peripheral blood mononuclear cells. Clinical & Experimental Immunology. 2005; 140: 478-490.
- Pilette C, Detry B, Guisset A, Gabriels J, Sibille Y. Induction of interleukin-10 expression through Fcalpha receptor in human monocytes and monocyte-derived dendritic cells: role of p38 MAPKinase. Immunol Cell Biol. 2010; 88: 486-493.
- Abolhassani H, Gharib B, Shahinpour S, Masoom SN, Havaei A, Mirminachi B, et al. Autoimmunity in patients with selective IgA deficiency. J Investig Allergol Clin Immunol. 2015; 25: 112-119.
- Singh K, Chang C, Gershwin ME. IgA deficiency and autoimmunity. Autoimmun Rev. 2014; 13: 163-177.
- Janzi M, Kull I, Sjöberg R, Wan J, Melén E, Bayat N, et al. Selective IgA deficiency in early life: association to infections and allergic diseases during childhood. Clin Immunol. 2009; 133: 78-85.
- Domínguez O, Giner MT, Alsina L, Martín MA, Lozano J, Plaza AM. Clinical phenotypes associated with selective IgA deficiency: a review of 330 cases and a proposed follow-up protocol. An Pediatr (Barc). 2012; 76: 261-267.
- Wang N, Lu P, Ling B, Zhu Z, Hammarström L. Caucasian origin of disease associated HLA haplotypes in chinese blood donors with IgA deficiency. J Clin Immunol. 2014; 34: 157-162.
- Al-Attas RA, Rahi AH. Primary antibody deficiency in Arabs: first report from eastern Saudi Arabia. J Clin Immunol. 1998; 18: 368-371.
- Gloudemans AK, Lambrecht BN, Smits HH. Potential of immunoglobulin A to prevent allergic asthma. Clinical and Developmental Immunology. 2013; 11.
- Herrant M, Loucoubar C, Boufkhed S, Bassène H, Sarr FD, Baril L, et al. Risk factors associated with asthma, atopic dermatitis and rhinoconjunctivitis in a rural Senegalese cohort. Allergy Asthma Clin Immunol. 2015; 11: 24.
- Langen U, Schmitz R, Steppuhn H. Prevalence of allergic diseases in Germany: Results of the German Health Interview and Examination Survey for Adults (DEGS1). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013; 56: 698-706.
- Campisi G, Chiappelli M, De Martinis M, Franco V, Ginaldi L, Guiglia R, et al. Pathophysiology of age-related diseases. Immun Ageing. 2009; 6:12.
- De Martinis M, Sirufo MM, Ginaldi L. Allergy and Aging: An old/new emerging health issue. Aging Dis. 2017; 8: 162-175.
- Amaral AFS, Newson RB, Abramson MJ, Antó JM, Bono R, Corsico AG, et al. Changes in IgE sensitization and total IgE levels over 20 years of follow-up. J Allergy Clin Immunol. 2016; 137: 1788-1795.
- Droste JH, Kerhof M, De Monchy JG, Schouten JP, Rijcken B. Association of skin test reactivity, specific IgE, total IgE, and eosinophils with nasal symptoms in a community-based population study. The Dutch ECRHS Group J Allergy Clin Immunol. 1996; 97: 922-932.
- Kerkhof M, Droste JH, De Monchy JG, Schouten JP, Rijcken B. Distribution of total serum IgE and specific IgE to common aeroallergens by sex and age, and their relationship to each other in a random sample of the Dutch general population aged 20-70 years. Dutch ECRHS Group, European Community Respiratory Health Study. Allergy. 1996; 51: 770-776.
- Omenaas E, Bakke P, Elsayed S, Hanoa R, Gulsvik A. Total and specific serum IgE levels in adults: relationship to sex, age and environmental factors. Clin Exp Allergy. 1994; 24: 530-539.
- Custovic A, Soderstrom L, Ahlstedt S, Sly PD, Simpson A, Holt PG. Allergen-specific IgG antibody levels modify the relationship between allergen-specific IgE and wheezing in childhood. J Allergy Clin Immunol. 2011; 127: 1480-1485.
- Culver EL, Sadler R, Bateman AC, Makuch M, Cargill T, Ferry B, et al. Increases in IgE, eosinophils, and mast cells can be used in diagnosis and to predict relapse of IgG4-related disease. Clin Gastroenterol Hepatol. 2017; 15: 1444-1452.
- Lilja G, Magnusson CG, Kusoffsky E, Johansson SG, Oman H. Neonatal IgA and IgE levels among infants with paternal heredity for atopic disease. Allergy. 1995; 50: 723-728.
- Ledford DK. Increased IgE in IgA deficiency. J Allergy Clin Immunol Pract. 2017; 20: S2213-S2198
- Smith JK, Krishnaswamy GH, Dykes R, Reynolds S, Berk SL. Clinical manifestations of IgE hypogammaglobulinemia. Ann Allergy Asthma Immunol. 1997; 78: 313-318.
- Levy Y, Nakum A, Segal N, Monselise Y, Danon YL. The association of selective IgA deficiency and IgE hypogammaglobulinemia. Allergy. 2005; 60: 836-838.
- Stoica G, Macarie E, Michiu V, Stoica RC. Biologic variation of human immunoglobulin concentration. I. Sex-age specific effects on serum levels of IgG, IgA, IgM and IgD. Med Interne. 1980; 18: 323-332.
- Viktorin A, Frankowiack M, Padyukov L, Chang Z, Melén E, Sääf A, et al. IgA measurements in over 12 000 Swedish twins reveal sex differential heritability and regulatory locus near CD30L. Hum Mol Genet. 2014; 23: 4177-4184.
- Weber-Mzell D, Kotanko P, Hauer AC, Goriup U, Haas J, Lanner N, et al. Gender, age and seasonal effects on IgA deficiency: a study of 7293 Caucasians. Eur J Clin Invest. 2004; 34: 224-228.
- Viktorin A, Frankowiack M, Padyukov L, Chang Z, Melén E, et al. Magnusson. IgA measurements in over 12 000 Swedish twins reveal sex differential heritability and regulatory locus near CD30L. Hum Mol Genet. 2014; 23: 4177-4184.
- Stoica G, Macarie E, Michiu V, Stoica RC. Biologic variation of human immunoglobulin concentration. I. Sex-age specific effects on serum levels of IgG, IgA, IgM and IgD. Med Interne. 1980; 18: 323-332.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.