Effect of Methotrexate Therapy on p53 and Bcl2 Expression in Patients with Psoriasis: A Prospective Hospital-Based Cohort Study
1 Department of Dermatology, Himalayan Institute of Medical Sciences, Swami Rama Himalayan University, Jolly Grant, Dehradun, Uttarakhand, India
2 Department of General Medicine, Himalayan Institute of Medical Sciences, Swami Rama Himalayan University, Jolly Grant, Dehradun, Uttarakhand, India
Citation: Kalyan S, et al. Effect of Methotrexate Therapy on p53 and Bcl2 Expression in Patients with Psoriasis: A Prospective Hospitalbased Cohort Study. Ann Med Health Sci Res. 2018;8:84-89
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Psoriasis is a chronic, relapsing, inflammatory, and hyperproliferative skin disease. The growth of keratinocytes is regulated by a delicate balance between molecules controlling cell survival (such as Bcl2) and cell death (such as p53). The study was conducted to observe the clinical and histopathological effect of Methotrexate on psoriatic lesions. Materials & Methods: The immunohistochemical expression of pro-apoptotic (p53) and anti-apoptotic (Bcl2) proteins was correlated with histomorphological changes (epidermal thickness, munro microabscess, granular layer, lymphocytic infiltrate, blood vessels) in the psoriatic skin. Results: A total of 35 cases of psoriasis were studied. Male predominance was seen and trunk was the initial site of involvement in 40% cases. There was a significant reduction in PASI (Psoriasis Area Severity Index) score, grade 3 cases of psoriasis and mean expression of p53 in all the histomorphological parameters in the subsequent 2 and 6 weeks of methotrexate therapy. The expression of p53 in all parameters and Bcl2 in the lymphocytes is significantly higher (p <0.05) in psoriatic skin as compared to the normal skin (control group). Conclusion: Low dose of methotrexate (0.3-0.5 mg/kg) contribute to reduction in epidermal thickness and thereby remain an effective therapy for psoriasis.
Keywords
Hyperproliferative; Apoptosis; Biopsy; Post treatment
Introduction
Psoriasis is a primary inflammatory disorder induced and sustained by skin infiltrating lymphocytes with a secondary striking proliferation of keratinocytes and epidermal hyperplasia. The word “psoriasis” comes from Greek word meaning “the state of having the itch”. [1] It affects about 2% of the world population with a bimodal age distribution (<30 years and > 50 years). [2] The disease occurs equally in both sexes; Indian males however are affected twice as frequently as females and the prevalence in the country varies from 0.44 to 2.8%. [3]
Psoriasis, a hyperproliferative keratinocytic disease, demonstrates a disturbance in equilibrium between the molecules controlling cell survival (such as Bcl2) and cell death (such as p53). [4] Although there is no cure for psoriasis but several treatments can minimize the disease and some can also induce remission of months to years. Treatment modalities evaluated and approved for the same are methotrexate, cyclosporine, acitretin, infliximab, itolizumab, erlotinib, Narrow band-Ultraviolet B (NB-UVB) phototherapy and PUVA (Psoralen plus Ultraviolet A) phototherapy etc. either alone or in combination. [5]
Methotrexate is an economical and effective antipsoriatic agent. It exerts an anti-mitotic action on psoriatic skin by competitively inhibiting dihydrofolate reductase and hence DNA synthesis. [6]
It also prevents cell entry into the S phase and causes killing of further cells. [7]
Literature on the effect of methotrexate therapy on the histological features in psoriatic lesions is limited. We undertook the present study to evaluate the impact of methotrexate on the expression of pro-apoptotic (p53) and anti-apoptotic (Bcl2) proteins and correlate it with the histomorphological features (epidermal thickness, munro microabscess, lymphocytic infiltrate etc.) in psoriatic lesions.
Methods
The prospective study was conducted on a cohort of patients with psoriasis attending a tertiary referral center of North India over a period of 12 months. Institutional ethical clearance was obtained and the patients were included following a written informed consent. Histologically proven psoriasis and treatment naïve patients of all ages (defined as not having received any topical or systemic therapy for psoriasis in the form of methotrexate/ retinoids/ phototherapy/ other immuno-suppressive agents in the last 6 months) were included and the pretreatment status was designated as day 0.
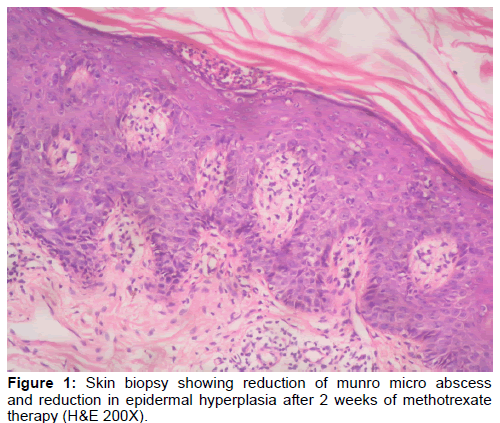
All included patients were administered methotrexate (0.3-0.5 mg/kg of body weight/week, depending on disease severity) and biopsy was taken from the same site subsequently on the 14th day and at the end of 6th week of starting the therapy. Harris Hematoxylin and Eosin stain (H&E) was used and histopathological characteristics viz. Munro microabscesses, spongiform pustules, epidermal hyperplasia, parakeratosis, abnormal granular layer, dilated blood vessels and lymphocytic infiltrate in dermis were studied and graded. Each characteristic was graded as 0-3 (nil to marked) using a visual analog scale.
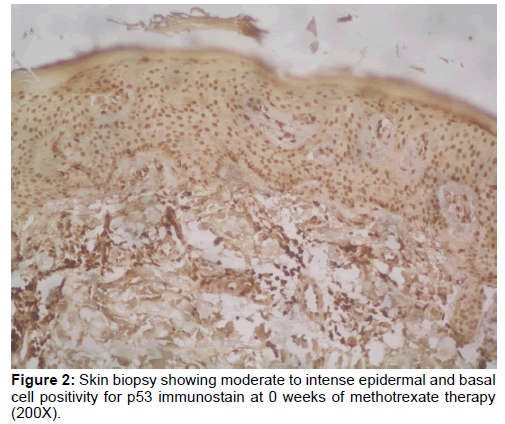
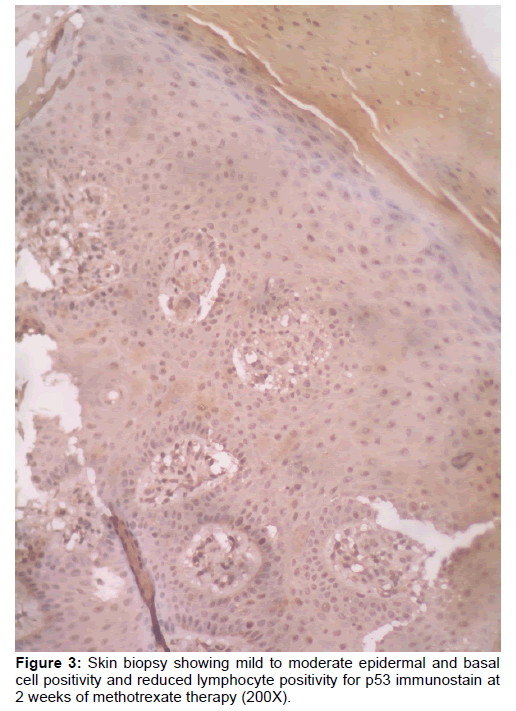
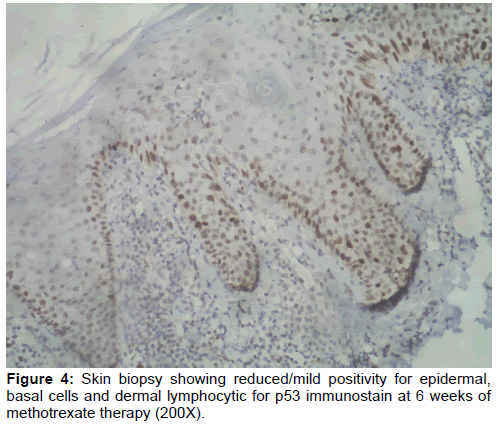
Monoclonal mouse antibodies for p53 (clone-DO7) and Bcl2 (clone-Bcl2/100) [manufactured by Bio SB] were used for immunohistochemistry and scoring was done as per the system devised by Liang et al. [8] Localization of immunohistochemical staining was categorized as epidermal, basal cell and lymphocyte staining. Basal cell staining was evaluated separately from epidermal cell staining because of the differences in the kinetics of the epidermal cells.
A group of age and sex matched controls (n=35) was also studied for p53 and Bcl2 expression in non-psoriatic skin lesions with an intention to validate the importance of these proteins in psoriasis. The Psoriasis Area and Severity Index (PASI) score was used as a measure of the severity of psoriatic lesions based on area coverage and plaque appearance. [9] This score was recorded in every visit prior to biopsy.
Statistical analysis
Statistical analysis was performed using the commercially available SPSS version 20. Qualitative data (munro microabscess, epidermal thickness, p53 and Bcl2 expression score etc.) was expressed as frequency and/or percentage. Quantitative data (age, PASI score) was represented in the form of mean ± SD. Paired t test was used to compare the mean of PASI score before and after methotrexate therapy. Wilcoxon signed rank test was used to compare the mean histomorphological features and immunostain expression score before and after therapy. Friedman test was done to compare the sequential change in histomorphological features and immunostain expression score from 0 week to 2 weeks and 6 weeks of therapy. Mann-Whitney U test was used to compare the immunostain expression score in normal epidermis and psoriatic epidermis. A p value < 0.05 was considered as significant.
Results
Of the 35 cases of psoriasis studied, 12 (34.3%) were in the 3rd to 4th decade (range 18-65 years). The mean age at diagnosis was 37.1 years and the male to female ratio was 3.35:1. All the patients presented with erythema and scaling while 94.3% (n=33) complained of itching additionally. Trunk was the most common site of involvement (n=14, 40%) followed by scalp and lower limb in equal number of cases (n=8, 22.9%); extra-cutaneous involvement was seen in 16 (45.7%) patients. Cold weather in winters aggravated the symptoms in 29 cases (82.9%). The histomorphological features studied showed a serial and significant reduction from the baseline [Table 1]. The reduction was progressive at 2 and 6 weeks of methotrexate therapy. Likewise, the PASI score showed a significant reduction from the baseline that was maintained at 2 and 6 weeks (18.25 ± 8.84 vs.10.11 ± 5.75 vs. 5.06 ± 3.71; p<0.05). However, complete clearance of PASI was not observed in any patient during the study period. The reduction was seen even in patients with grade 3 psoriasis; grade 0 psoriasis increased after methotrexate therapy.
| Histomorphological features | 0 weeks (Mean ± SD) |
2 weeks (Mean ± SD) |
6 weeks (Mean ± SD) |
P` value between 0 weeks and 2 weeks | P` value between 0 weeks and 6 weeks | P° value |
|---|---|---|---|---|---|---|
| Munro microabscess | 2.29 ± 0.75 | 1.11 ± 0.63 | 0.77 ± 0.88 | <0.001 | <0.001 | <0.001 |
| Spongiform pustules | 1.89 ± 0.72 | 0.94 ± 0.59 | 0.60 ± 0.81 | <0.001 | <0.001 | <0.001 |
| Epidermal hyperplasia | 2.66 ± 0.48 | 1.91 ± 0.56 | 1.49 ± 0.85 | <0.001 | <0.001 | <0.001 |
| Parakeratosis | 2.40 ± 0.65 | 1.26 ± 0.66 | 0.94 ± 0.91 | <0.001 | <0.001 | <0.001 |
| Abnormal granular layer | 2.17 ± 0.82 | 1.31 ± 0.63 | 0.97 ± 0.82 | <0.001 | <0.001 | <0.001 |
| Dilated blood vessels | 1.57 ± 0.61 | 1.23 ± 0.43 | 0.89 ± 0.58 | 0.007 | <0.001 | <0.001 |
| Lymphocytic infiltrate | 2.03 ± 0.66 | 1.46 ± 0.56 | 1.31 ± 0.53 | <0.001 | <0.001 | <0.001 |
P` value by Wilcoxon signed rank test; P° value by Friedman test
Table 1: Skin biopsy showing reduction of munro micro abscess and reduction in epidermal hyperplasia after 2 weeks of methotrexate therapy (H&E 200X).
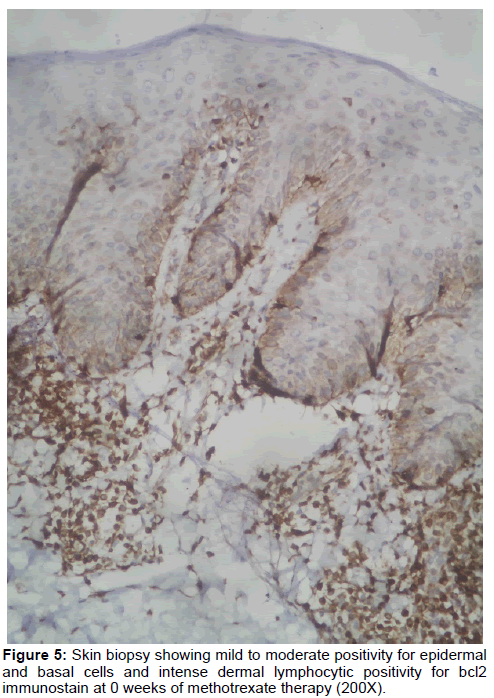
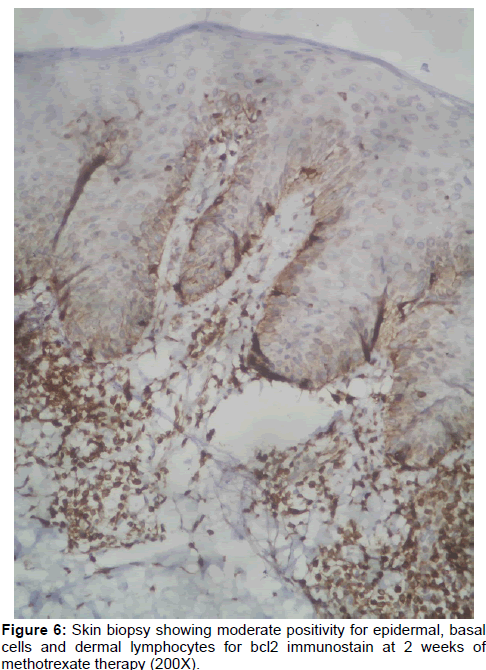
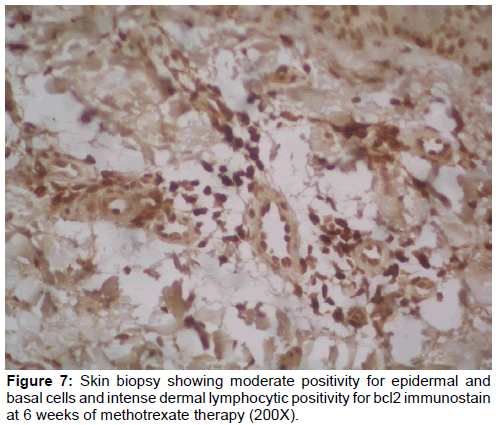
The expression of Bcl2 in the lymphocytes was significantly higher (p<0.05) as was the p53 expression in all cell types (i.e. epidermal, basal cells and lymphocytes) in psoriatic skin as compared to the non-psoriatic control group; Bcl2 expression in epidermal and basal cells was comparable in the two groups [Tables 2 and 3] [Figures 1 - 7].
| p53 expression | Control | 0 weeks (Mean ± SD) |
2 weeks (Mean ± SD) |
6 weeks (Mean ± SD) |
P value between control and psoriatic patients at 0 weeks |
P` value between 0 weeks and 2 weeks |
P` value between 2 weeks and 6 weeks |
P° value |
|---|---|---|---|---|---|---|---|---|
| Epidermal cells | 1.4± 0.84 | 3.26 ± 0.74 | 2.74 ± 0.66 | 2.40 ± 0.74 | <0.001 | 0.006 | <0.001 | <0.001 |
| Basal cells | 2.4± 0.70 | 4.14 ± 0.88 | 3.74 ± 0.98 | 3.17 ± 1.01 | <0.001 | 0.032 | <0.001 | <0.001 |
| Lymphocytes | 2.3± 0.68 | 3.31 ± 1.08 | 3.14 ± 0.94 | 2.46 ± 0.66 | 0.006 | 0.450 | 0.001 | <0.001 |
P value by Mann- Whitney U test (2-tailed value); P` value by Wilcoxon signed rank test; P° value by Friedman test
Table 2: p53 expression in psoriatic skin at 0 weeks, 2 weeks and 6 weeks of methotrexate therapy.
| Bcl2 expression | Control | 0 weeks (Mean ± SD) |
2 weeks (Mean ± SD) |
6 weeks (Mean ± SD) |
P value between control and psoriatic patients at 0 weeks | P` value between 0 weeks and 2 weeks | P` value between 2 weeks and 6 weeks | P° value |
|---|---|---|---|---|---|---|---|---|
| Epidermal cells | 2.60±0.70 | 3.03 ± 0.86 | 3.06 ± 1.0 | 3.00 ± 0.87 | 0.182 | 0.966 | 0.925 | 0.972 |
| Basal cells | 3.70±0.68 | 4.00 ± 0.80 | 4.34 ± 1.08 | 3.80 ± 1.02 | 0.158 | 0.090 | 0.327 | 0.077 |
| Lymphocytes | 3.67±0.70 | 4.43 ± 0.85 | 4.34 ± 1.37 | 4.26 ± 1.27 | 0.005 | 0.989 | 0.437 | 0.918 |
P-value by Mann- Whitney U-test (2-tailed value); P` value by Wilcoxon signed rank test; P° value by Friedman test
Table 3: Bcl2 expression in psoriatic skin at 0 weeks, 2 weeks and 6 weeks of methotrexate therapy.
Discussion
The expression of the pro-apoptotic p53 protein was higher while that of the anti-apoptotic Bcl2 protein was lower in psoriatic lesions as compared to non-psoriatic lesions. Methotrexate had a positive effect on the histomorphological features of psoriatic lesions. The effect was pronounced and sustained on p53 over a period of 6 weeks.
More than two-third of our patients were between 31-50 years; however, Okhandiar et al reported the highest incidence in the second decade of life. The apparent reason for this was the large number of subjects (n=3573). [10] Likewise, the high male: female ratio in the present study in comparison to 2.46:1, 2.40:1 and 2.03:1 reported in other studies may be attributable to the variable sample sizes. [9,11,12] The symptoms of scaling and itching are concordant with the previous study by Prignano et al. [13]
Trunk, an uncommon site for psoriatic lesions was observed in 40% of our subjects. The reduction in the mean PASI score was similar to that observed in the studies by Yazici et al and Saurat et al after 6 and 16 weeks of treatment with methotrexate respectively. [14,15]
The characteristic pattern of fully developed psoriasis includes elongation of rete pegs leading to regular acanthosis, edema of the papillary dermis associated with tortuous dilated vessels, thinning of suprapapillary area, decreased thickness of granular layer and exocytosis of neutrophils in the spinous layer (kogoj’s pustule) or in the cornified parakeratotic layer (munro microabscesses). [16] Yazici et al. found a decrease in inflammatory cell infiltrate and progressive loss of elongated rete pegs with the return of a normal stratum corneum in patients after 6 weeks of methotrexate therapy. [14] In our study, we found that there was an increase in grade 0 cases and a significant reduction in grade 3 cases of psoriasis in all the histomorphological parameters over 0 week to subsequent 2 and 6 weeks.
El-Batawi et al. in a study on expression of Bcl2 and p53 in psoriasis found higher p53 expression in lesional than in non lesional psoriatic skin using monoclonal antibody Do7. They concluded that elevated levels of p53 in psoriatic plaques reflect an important role exerted by this tumor suppressor gene on the development of psoriatic plaques. [17] Hussein et al. showed that the Bcl2 score in epidermal keratinocytes in normal skin is slightly higher (0.70 ± 0.26) as compared to the psoriatic skin (0.46 ± 0.22) and in inflammatory cells in normal skin, it is lower (2.00 ± 0.00) as compared to the psoriatic skin (3.00 ± 0.39). [18] El-Domyati et al. found that in psoriatic plaques, Bcl2 was expressed in the keratinocytes of 23.3% cases (mean, 0.3 ± 0.6) and in the lymphocytes of 56.67% cases (mean, 0.8 ± 0.8). In non lesional skin, Bcl2 was expressed in keratinocytes in 46.67% cases (mean, 0.6 ± 0.6) but was not detected in the lymphocytes. The expression was not significantly different in keratinocytes but significantly higher in lymphocytes. [19] Our results are concordant with the results of few studies and show that Bcl2 was moderately expressed in the control group in epidermal cells (mean, 2.6 ± 0.70), basal cells (Mean, 3.7 ± 0.68) and lymphocytes (mean, 3.67 ± 0.70). At 0 weeks in psoriatic patients, Bcl2 was moderately expressed in epidermal cells (mean, 3.03 ± 0.86) and strongly expressed in basal cells (mean, 4.00 ± 0.80) and lymphocytes (Mean, 4.43 ± 0.85). The expression of Bcl2 in the lymphocytes is significantly higher (p<0.05) in psoriatic skin as compared to the normal skin (control group) but the difference in Bcl2 expression in epidermal and basal cells is statistically insignificant. In the present study, mean expression of Bcl2 in epidermal cells, basal cells and lymphocytes showed significant reduction neither after 2 weeks (p>0.05) nor after 6 weeks (p>0.05) of methotrexate therapy in all the three parameters, keeping 0 week as the baseline.
Some studies have been conducted to look for histological and immunohistochemical changes after giving treatment either in the form of phototherapy or drugs like acitretin, PUVA, [19] calcipotriol, [20] infliximab, [21] anthralin or aloe vera [21] but very few have been done using methotrexate [Table 4]. [5]
| Parameters | Adisen et al.[19] using calcipotriol and methylprednisolone (2005) | Gomez et al.[20] using Infliximab (2009) | Domyati et al.[18] using PUVA therapy (2012) | El Gayyar et al.[21] using aloe vera and coal tar mixture (2012) | Present study using methotrexate (2017) | |
|---|---|---|---|---|---|---|
| Epidermal thickness | - | ↓ | significant ↓ (p<0.001) | - | significant ↓(p<0.001) | |
| Munro microabscess | - | ↓ | - | - | significant ↓(p<0.001) | |
| Spongiform pustules | - | ↓ | - | - | significant ↓(p<0.001) | |
| Dermal inflammatory infiltrate | - | ↓ | - | significant↓ (p<0.001) | ||
| P53 expression | Epidermal cells | significant ↓ with both (p<0.05) | significant ↓ (p<0.05) | significant ↑ (p<0.001) | - | significant↓ (p<0.001) |
| Basal cells | - | - | - | - | significant↓(p<0.001) | |
| Lymphocytes | - | - | No significant difference | - | significant ↓(p<0.001) | |
| Bcl2 expression | Epidermal cells | significant ↑ with both (p<0.05) | negative | significant↑ (p<0.001) | significant↓ (p<0.01) | Insignificant (p=0.972) |
| Basal cells | - | - | - | - | Insignificant (p=0.077) | |
| Lymphocytes | - | - | Significant ↓ (p=0.01) | ↓but insignificant (p>0.05) | Insignificant (p=0.918) | |
Table 4: Comparison of previous studies using various therapeutic modalities for psoriasis with present study using methotrexate.
In the present study, histomorphology and expression of p53 and Bcl2 before and after methotrexate therapy in psoriatic patients was studied. All the histomorphological parameters were reduced significantly (p<0.05) after methotrexate therapy. There was also a significant reduction (p<0.05) in p53 expression in epidermal cells, basal cells and lymphocytes. But the expression of Bcl2 was variable in all the three parameters. We can thus safely say that low dose of methotrexate (0.3-0.5 mg/kg) contributes to reduction in epidermal thickness and thereby remains an effective therapy for psoriasis.
Conflict of Interest
All authors disclose that there was no conflict of interest
REFERENCES
- Ram S. Indian psoriasis research: An impact assessment through bibliometric studies. J Scientometric Res 2013;2:126-31.
- Magela GM, Coelho SD, Do Amaral Peisino K, Machado-Pinto J, Cuzzi T. Psoriasis and pentoxifylline: a clinical, histopathologic, and immunohistochemical evaluation. Skinmed. 2006;5:278-84.
- Dogra S, Yadav S. Psoriasis in India: prevalence and pattern. Ind J Dermatol, Venereol and Leprol 2010;76:595-601.
- Hussein MR, Al-Badaiwy ZH, Guirguis MN. Analysis of p53 and bcl-2 protein expression in the non-tumorigenic, pretumorigenic, and tumorigenic keratinocytic hyperproliferative lesions. J Cutan Pathol 2004;31:643-651.
- Moradi TS, Taheri A, Alinia H, Mansoori P, Feldman S, Sandoval L. Emerging treatment options for psoriasis. Psoriasis: Targets and Therapy 2014;4:27-35.
- Haider S, Wahid Z, Najam Us S, Riaz F. Efficacy of Methotrexate in patients with plaque type psoriasis. Pak J Med Sci 2014;30:1050-1053.
- Heenen M, Laporte M, Noel JC, De Graef C. Methotrexate induces apoptotic cell death in human keratinocytes. Arch Dermatol Res 1998;290:240-245.
- Liang SB, Ohtsuki Y, Furihata M, Takeuchi T, Iwata J, Chen BK, et al. Sun-exposure-and aging-dependent p53 protein accumulation results in growth advantage for tumour cells in carcinogenesis of nonmelanocytic skin cancer. Virchows Archiv 1999;434:193-199.
- Fredriksson T, Pettersson U. Severe psoriasis--Oral therapy with a new retinoid Dermatologica 1978;157:238-244.
- Okhandiar R, Banerjee B. Psoriasis in the tropics: An epidemiological survey. J Ind Med Assoc 1963;41:550-556.
- Bedi T. Clinical profile of psoriasis in North India. Ind J Dermatol Venereol and Leprol 1995;61:202.
- Kaur I, Handa S, Kumar B. Natural history of psoriasis: a study from the Indian subcontinent. J Dermatol 1997;24:230-234.
- Prignano F, Ricceri F, Pescitelli L, Lotti T. Itch in psoriasis: epidemiology, clinical aspects and treatment options. Clin Cosmet Investig Dermatol 2009;2:9-13.
- Yazici AC, Tursen U, Apa DD, Ikizoglu G, Api H, Baz K, et al. The changes in expression of ICAM-3, Ki-67, PCNA, and CD31 in psoriatic lesions before and after methotrexate treatment. Arch Dermatol Res 2005;297:249-255.
- Saurat JH, Stingl G, Dubertret L, Papp K, Langley RG, Ortonne JP, et al. Efficacy and safety results from the randomized controlled comparative study of adalimumab vs. methotrexate vs. placebo in patients with psoriasis (CHAMPION). British J Dermatol 2007;158:558-566.
- Cribier B. Psoriasis under the microscope. J European Acad Dermatol Venereol 2006;20:3-9
- El Batawi M, Shahin Z, Ramadan S. Expression of Bcl-2 and P53 in psoriasis. Egypt J Dermatol Androl 2002;22:13-17.
- El-Domyati M, Moftah NH, Nasif GA, Abdel-Wahab HM, Barakat MT, Abdel-Aziz RT. Evaluation of apoptosis regulatory proteins in response to PUVA therapy for psoriasis. Photodermatology, Photoimmunology & Photomedicine 2013;29:18-26.
- Adisen E, Gulekon A, Erdem O, Dursun A, Gurer MA. The effects of calcipotriol and methylprednisolone aseponate on Bcl-2, p53 and ki-67 expression in psoriasis. J European Acad Dermatol Venereol 2006;20:527-533.
- Gómez-Mateo C, Avalos-Peralta S, Ríos-Martín J, Carrizosa-Esquivel A, González-Cámpora R, Camacho-Martínez F. Sequential histological and immunohistochemical assessment of proliferation and apoptotic markers during treatment of psoriasis with antitumor necrosis factor α (Infliximab). Actas Dermo-Sifiliográficas (English Edition). 2009;100:420-424.
- El-Gayyar M, El-Hawwary A, Bakre N. Evaluation of therapeutic effects of Aloe vera: Coal tar mixture in psoriasis: An immunohistochemical study. Asian J Dermatol 2012;4:16-28.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.