Lumbosacral Chordomas: The Enigmatic and Dreaded Entity
Received: 08-Dec-2023, Manuscript No. amhsr-23-123023; Editor assigned: 10-Dec-2023, Pre QC No. amhsr-23-123023 (PQ); Reviewed: 27-Dec-2023 QC No. amhsr-23-123023; Revised: 04-Jan-2024, Manuscript No. amhsr-23-123023 (R); Published: 11-Jan-2024
Citation: Fayaz M. Lumbosacral Chordomas: The Enigmatic and Dreaded Entity. Ann Med Health Sci Res. 2024;13: 919-923
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: Primary tumours of the spine are rare, accounting for less than 5% of all osseous neoplasms and less than 0.2% of all cancers. Among all primary tumours of the spine, the incidence of primary malignant tumours varies between 32% and 71%. The most common primary malignant tumours of the spine are chordoma and sacral sarcomas like chondrosarcoma, osteosarcoma and Ewing sarcoma. Chordoma is a slow-growing, locally aggressive neoplasm of bone which arises from embryonic remnants of the notochord, with an overall incidence of 0.08 per 100,000 individuals accounting for 40% of all primary sacral tumours. The tumour has a delicate pseudo capsule, in which satellite lesions and occult extension are frequent. Hence, local recurrence is expected due to failure to achieve negative surgical margins. Chordomas are insensitive to chemotherapy and radiotherapy. Therefore, complete surgical excision is the mainstay for long-term survival.
Materials and Methods: The present study was undertaken in the Department of Neurosurgery, Sher-i-Kashmir Institute of Medical Sciences. Our study was a prospective and retrospective study which included all patients who underwent surgical procedures for lumbosacral spinal chordomas, retrospectively from January 2008-August 2016 and prospectively from September 2016 to August 2018.
Results: Shows the age distribution of patients in study.Mean age was 53 years. Youngest patient was 18 years and eldest was 72 years. Maximum number of patients (33.33%) belonged to 50-60 age group, followed by 27.77% patients in age group of 60-70. Out of 18 patients 12 (66.6%) were males and 6 (33.3%) were females with a male to female ratio of 2:1. The symptomatology of the patients and the most common symptom was pain in 16 (89%) patients followed by weakness in 11 (61%) patients, followed by swelling in 11 (44%). Normal Power (grade V) power was present in 7 (38.8%) patients whereas powerwas decreased (grade III/IV) in 11 (61.11%) patients. The duration of symptoms is usually long due to vague symptomatology of the spinal chordomas. Patients often are seen in general surgery and urology specialities due to rectal dysfunction or urinary tract symptoms.In our study mean duration of symptoms before the patient was diagnosed was 24.88 months. Location of tumour in our study and tumour was sacral/ sacrococcygealin 13 (72%) and lumbar/lumbosacral in 5 (28%) of patients. Size of tumour ranged from 6 to 13 cm and mean greatest diameter was 9.8 cm. In our study, 55.5% of the patients had tumour size less than 10 cm whereas in 44.5% partients tumour size was greater than 10 cm. Out of 18 patients 16.6% patients had postoperative stay in hospital for 0-5 days, 27.8% patients had hospital stay for 5-10 days, 33.4% patients had stay in hospital for 10-15 days, 11.2% had stay in hospital for 15-20 days, 5.5% had stay in hospital for 25-30 days and 5.5% had hospital stay for 40-45 days and Range was between 5-41 days and mean duration of hospital stay was 13 days. Adjuvant therapy in the form of radiotherapy was given in 6 (33%) out of 18 patients.
Conclusions: Local recurrence of the disease was found in 7 (39%) out of 18 patients after a period of one year after surgery and within 3 years of follow up. Two patients had recurrence in 2nd year post surgery and five patients had recurrence in 3rd year after surgery. Metastasis was present in 3 (17%) of patients which included lung and bone metastasis.
Keywords
Chordoma; Tumour; Radiotherapy
Introduction
Primary tumours of the spine are rare, accounting for less than 5% of all osseous neoplasms and less than 0.2% of all cancers [1,2]. Among all primary tumours of the spine, the incidence of primary malignant tumours varies between 32% and 71% [3,4]. The most common primary malignant tumours of the spine are chordoma and sacral sarcomas like chondrosarcoma, osteosarcoma and Ewing sarcoma [5]. Chordoma is a slowgrowing, locally aggressive neoplasm of bone which arises from embryonic remnants of the notochord, with an overall incidence of 0.08 per 100,000 individuals accounting for 40% of all primary sacral tumours [6]. The male-female prevalence ratio is 2:1, with increasing incidence after the fourth decade [7]. The most common site of chordoma is the sacrum and coccyx (50%), followed by the skull base (30%) and vertebral bodies (20%) [8]. Chordomas are low to intermediate-grade malignant lesions. They may present with symptoms of bowel dysfunction or urinary tract symptoms. Neurogenic bowel dysfunction is a manifestation of bowel dysfunction resulting from sensory and motor disturbances due to neurological disease or damage, and its main symptoms include constipation, faecal incontinence, evacuation difficulties or a combination of these [9].
As chordomas have deep-seated locations in the pelvis with indolent and vague symptoms, they are significant often diagnosed late. They are usually large at diagnosis, involving adjacent neurovascular structures and vital organs in the pelvis. Chordoma expands in the sacral foramina and plugs the cephalad into the neural canal. Anteriorly it is usually contained by the presacral fascia, so the invasion of the rectal wall is not common. Posteriorly and laterally, it invades the gluteus maximus and piriformis muscles, sacroiliac joints, ligaments and subcutaneous fat. The confirmative diagnosis of chordoma, like other tumours, is histopathological. However, radiological evaluation of the patient is critical to look for the tumour size, underlying bone destruction, soft tissue involvement and metastases. A plain X-ray may show bone destruction or intervertebral space widening, CT findings suggestive are expansile lesion, bone destruction, calcification, and MRI findings are iso to hypointense on T1 and hyperintense on T2 images and helps define soft tissue extension or involvement [10]. The tumour is usually Enneking stage IB at diagnosis, and its large size, proximity to neurovascular structures, and congested pelvic structure make complete or wide tumour excision difficult. Also, larger and more proximally located tumours may require excision of sacral nerve roots leading to incontinence, sexual dysfunction and motor weakness. Metastases are not typical and occur late during the disease in the lung, bone, soft tissue, lymph node, liver and skin [11]. The tumour has a delicate pseudo capsule, in which satellite lesions and occult extension are frequent. Hence, local recurrence is expected due to failure to achieve negative surgical margins. Chordomas are insensitive to chemotherapy and radiotherapy. Therefore, complete surgical excision is the mainstay for long-term survival.
Materials and Methods
The present study was undertaken in the Department of Neurosurgery, Sher-i-Kashmir Institute of Medical Sciences. It is a retro-prospective observational study, which included all patients who underwent surgical procedures for lumbosacral spinal chordomas retrospectively from January 2008-August 2016 and prospectively from September 2016 to August 2018. The minimum follow-up period was six months, and the maximum was four years. Analysis was done regarding demographic data, clinical profile of patients, assessed for postoperative complications and follow-up for recurrence assessment and metastasis.
Results
The study included 18 patients, 12 males and six females, with a 2:1 ratio. The average age of presentation was 53 years (range 18-72 years). The maximum cases were seen in the 50-60 age group. The most common symptom was pain or low backache, which was present in 16 (89%), followed by weakness in legs (61%) which is grade III/IV, swelling (44%), bowel dysfunction (39%) and bladder symptoms (11%). Table 1 shows the demographics and clinical profile of the study population.
| Age(years) | N | |
|---|---|---|
| 01-Oct | 0 | |
| Oct-20 | 2 | |
| 20-30 | 1 | |
| 30-40 | 1 | |
| 40-50 | 2 | |
| 50-60 | 6 | |
| 60-70 | 5 | |
| Demographic | 70-80 | 1 |
| Total | 18 | |
| Mean | 53 Years. | |
| Range | 18-72 Years. | |
| Gender | N | % |
| Male | 12 | 66.66 |
| Female | 6 | 33.33 |
| Symptoms | N | % |
| Pain | 16 | 89 |
| Weakness of legs | 11 | 61 |
| Swelling | 8 | 44 |
| Bowel dysfunction | 7 | 39 |
| Bladder symptoms | 2 | 11 |
Table 1: Showing the demographics and clinical profile of study population.
The mean duration between the onset of symptoms and presentation was 24.88 months.
The tumour's location was lumbar/lumbosacral in 5 (28%) and sacral/sacrococcygeal in 13 (72%) patients. The size of the tumour ranged from 6 to 13 cm, and the mean diameter of 9.8 cm (Table 2).
| Neurological grade | N | % |
|---|---|---|
| Grade III/IV | 11 | 61.11 |
| Grade V | 7 | 38.8 |
| No. of patients | Mean duration of symptoms | |
| 18 | Months | |
| Site/ Location | N | % |
| Lumbar/Lumbosacral | 5 | 28 |
| Sacral/Sacrococcygal | 13 | 72 |
| Range of tumour size | 6-13 cm | |
| Mean greatest diameter | 9.8 | |
| Tumour size | N | % |
| Number of Patients having size of Tumour<10 cm | 10 | 55.50% |
| Number of Patients having size>10 cm | 8 | 44.50% |
Table 2: Neurological Grade (Power), duration of symptom, location and size of tumour.
Ten patients have a tumour size of less than 10 cm, and eight have more than 10 cm.
All 18 patients underwent surgery. Most patients (33.4%) have hospital stays of 10-15 days, with a mean duration of 13 days. Adjuvant therapy was given in 6 patients (33%). Out of 18 patients, 9 had postoperative complications, which included CSF leak in 6 patients, wound infection in 8 patients, urinary incontinence in 2 patients and Deep Vein Thrombosis (DVT) in 1 patient. Tumour recurrence was seen in 7 patients (39%) and metastasis in 3 patients (17%) (Table 3).
| Duration of hospital stay: | No. of patients | Percentage |
|---|---|---|
| 0-5 days | 3 | 16.6 |
| 5-10 days | 5 | 27.8 |
| 10-15 days | 6 | 33.4 |
| 15-20 days | 2 | 11.2 |
| 20-25 days | 0 | 0 |
| 25-30 days | 1 | 5.5 |
| 30-35 days | 0 | 0 |
| 35-40 days | 0 | 0 |
| 40-45 days | 1 | 5.5 |
| Total=18 | 100 | |
| Adjuvant therapy | N | % |
| Given | 6 | 33 |
| Not Given | 12 | 67 |
| N | % | |
| Recurrence | 7 | 39 |
| No Recurrence | 11 | 61 |
| Metastasis | N | % |
| Present | 3 | 17 |
| Absent | 15 | 83 |
Table 3: Duration of hospital stay, Adjuvant Therapy, Local Recurrence and Metastasis.
Discussion
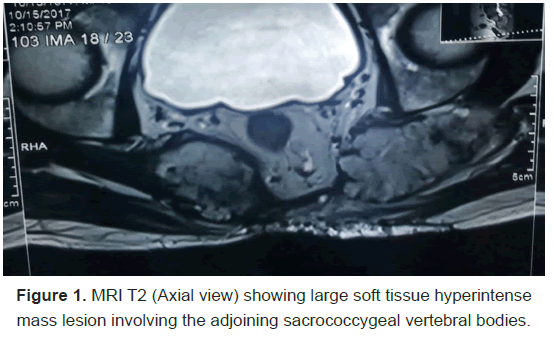
Chordoma is a primary malignant spinal tumour, accounting for less than 5% of all osseous neoplasms and less than 0.2% of all cancers [1,2]. It is a slow-growing, locally aggressive neoplasm of bone arising from embryonic remnants of the notochord. The overall incidence is 0.08 per 100,000 individuals accounting for 40% of all primary sacral tumours [6]. Ropper et al., in their study, found the male-to-female prevalence ratio is 2:1, with an increasing incidence after the fourth decade [7]. The male-tofemale ratio in our study was 2:1, which corresponds to most of the case series [7,8,12]. Ozger et al., in their research, described the mean age as 55.5 years. It is similar to our finding of 53 years mean age. Most of the chordomas are seen in the sacrococcygeal region (50%), skull base (30%) and 20% in the vertebral bodies. In our study, the tumour's location was lumbar/lumbosacral in 5 (28%) and sacral/sacrococcygeal in 13 (72%) patients as shown in Figure 1.
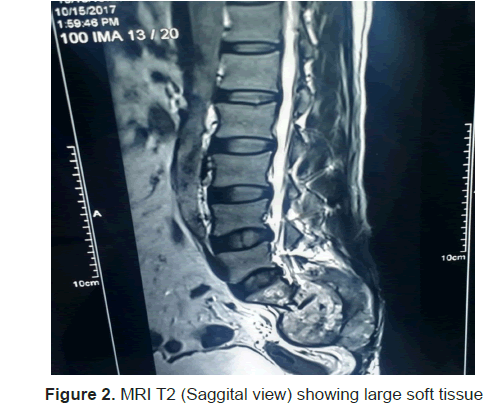
In our study, the most common symptom was pain or low backache, which was present in 16 (89%). This corresponds to other studies which describe the most common symptom as pain or low back ache [13-16]. The mean duration between the onset of symptoms and presentation in our study was 24.88 months, while the literature reported a range of 20 to 44.4 months [8,15]. The confirmative diagnosis of chordoma, like other tumours, is histopathological. However, radiological evaluation of the patient is critical to look for the tumour size, underlying bone destruction, soft tissue involvement and metastases. A plain X-ray may show bone destruction or intervertebral space widening, CT findings suggestive are expansile lesion, bone destruction, calcification, and MRI findings are iso to hypointense on T1 and hyperintense on T2 images and helps define soft tissue extension or involvement as shown in Figure 2.
We investigated our patients with all three modalities. Fuchs et al. reported a mean diameter of 9 cm in a series of 52 patients [17]. Ozger et al. reported a mean diameter of 10.7 cm in 17 patients [8]. In our study, the size of the tumour ranged from 6 to 13 cm, and the mean greatest diameter was 9.8 cm. The tumour was more significant than 10 cm in 8 (45%) of patients and less than 10 cm in 10 (55%) of patients.
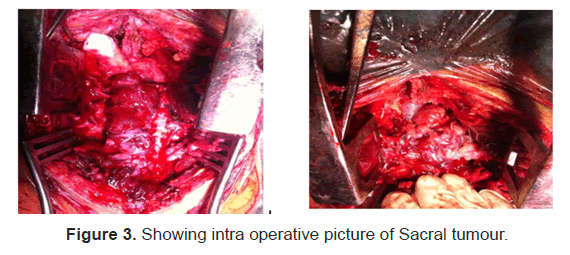
The management of spinal chordomas includes surgery, radiation therapy, and chemotherapy, with some future directions regarding treatment. For surgical treatment, either a combined anterior or posterior approach or a single posterior approach is used. The surgical plan depends on the size and the site of the tumour. If the tumour is more significant than 10 cm in its largest diameter, extends to the level of S2 and above, or invades intrapelvic structures anterior to the presacral fascia, irrespective of the site, a combined anteroposterior approach is used. If the tumour is smaller than 10 cm in its greatest diameter and only involves the lower sacrum and posterior muscles, a posterior-only approach is used. In our study, all patients underwent surgery with widemargin excision as shown in Figure 3. If the presacral fascia or rectal adventitia are infiltrated, the rectum is included in the surgical resection done in two patients [8,18]. Radiotherapy alone has long been recognised as ineffective means to treat chordomas; however, recent technological advances that allow for large radiation doses are beginning to change this sentiment, namely radiation treatment via hadrons high dose protons or other charged particles (e.g. carbon ions, helium or neon), has allowed for the local delivery of high doses while sparing nearby delicate neural structures. Relative to photon therapy, hadron therapy has demonstrated higher biological effectiveness and a smaller oxygen-enhancement ratio in the tumour area. Adjuvant treatment in the form of radiation is given in 6 patients (33%) in our study.
In our study, the mean duration of hospital stay, surgery to discharge, was 13 days. The patients with postoperative complications had more hospital stays. In our study, local recurrence was found in 7 (39%) of patients. Recurrence was seen within three years of follow-up. Two patients had recurrence one year after surgery (in 2nd year), and five patients had recurrence in the third year post-surgery. Out of these, the re-excision was done in 5 patients, and two were given radiotherapy only. The recurrence rate varies in the literature from 33 to 70% [8,12,17,19,20]. Ozger et al., reported a recurrence rate of 41%. Fuchs et al., in 2005 in their study described twentythree patients (44%) who had local recurrence [17]. Metastasis is uncommon and occurs late in the course of the disease in the lungs, bone, soft tissue, lymph node, liver and skin. The rate of metastasis varies from 10 to 43% in the literature [8,19,21]. The most frequent site of metastasis is the lung. Young et al., in 2015 in their study described 39 patients (17.8%) who developed metastatic disease, most frequently to the lung (>50%) [21].
Conclusion
Chordoma is a devastating and nagging tumour with insidious onset. The age of presentation is usually more than the 5th decade with males predominantly affected in the ratio of 2:1. Pain is the most typical symptom at exhibition. CT scan and MRI give a presumptive diagnosis of chordoma, which is confirmed by histopathological examination. Treatment is challenging and multi-pronged with surgery being the mainstay complemented by radiotherapy for recurrence and palliation.Treatment which may be complicated by postoperative complications like wound infection, CSF leak or bowel or bladder dysfunction.
References
- Venkateswaran L, Rodriguez-Galindo C, Merchant TE, Poquette CA, Rao BN, et al. Primary Ewing tumour of the vertebrae: Clinical characteristics, prognostic factors, and outcome. Med Pediatr Oncol. 2001;37:30–5.
[Crossref] [Google Scholar] [PubMed]
- Ruggieri P, Angelini A, Ussia G, Montalti M, Mercuri M. Surgical Margins and Local Control in Resection of Sacral Chordomas. Clin Orthop. 2010;468:2939.
[Crossref] [Google Scholar] [PubMed]
- Mukherjee D, Chaichana KL, Gokaslan ZL, Aaronson O, Cheng JS, et al. Survival of patients with malignant primary osseous spinal neoplasms: Results from the Surveillance, Epidemiology, and End Results (SEER) database from 1973 to 2003. J Neurosurg Spine. 2011;14:143–50.
[Crossref] [Google Scholar] [PubMed]
- Kelley SP, Ashford RU, Rao AS, Dickson RA. Primary bone tumours of the spine: A 42-year survey from the Leeds Regional Bone Tumour Registry. Eur Spine J. 2007;16:405–9.
[Crossref] [Google Scholar] [PubMed]
- Mukherjee D, Chaichana KL, Adogwa O, Gokaslan Z, Aaronson O, et al. Association of extent of local tumour invasion and survival in patients with malignant primary osseous spinal neoplasms from the surveillance, epidemiology, and results (SEER) database. World Neurosurg. 2011;76:580–5.
[Crossref] [Google Scholar] [PubMed]
- Smoll NR, Gautschi OP, Radovanovic I, Schaller K, Weber DC. Incidence and relative survival of chordomas: The standardised mortality ratio and the impact of chordomas on a population. Cancer. 2013;119:2029–37.
[Crossref] [Google Scholar] [PubMed]
- Ropper AE, Cahill KS, Hanna JW, McCarthy EF, Gokaslan ZL, et al. Primary vertebral tumours: A review of epidemiologic, histological and imaging findings, part II: Locally aggressive and malignant tumours. Neurosurgery. 2012;70:211–9; discussion 219.
[Crossref] [Google Scholar] [PubMed]
- Ozger H, Eralp L, Sungur M, Atalar AC. Surgical management of sacral chordoma. Acta Orthop Belg. 2010;76:243–53.
[Google Scholar] [PubMed]
- Kumar L, Athanasakos E, Emmanuel AV. Evaluation and Treatment of Neurogenic Bowel Dysfunction-A Review. Eur Neurol Rev. 2016.
- Swathi Vasanthi AVSS, Pravallika I, Kejriwal GS, Madhavi CH. Role of imaging in Chordoma with Histopathological correlation. International Journal of Current Research.
- Rohatgi S, Ramaiya N, Jagannathan J, Howard SA. Metastatic Chordoma: Report of the Two Cases and Review of the Literature. Eurasian J Med. 2015;47:151-4.
[Crossref] [Google Scholar] [PubMed]
- Kerekes D, Goodwin CR, Ahmed AK, Verlaan JJ, Bettegowda C, et al. Local and Distant Recurrence in Resected Sacral Chordomas: A Systematic Review and Pooled Cohort Analysis. Glob Spine J. 2019;9:191–201.
[Crossref] [Google Scholar] [PubMed]
- Atalar H, Selek H, Yildiz Y, Sağlik Y. Management of sacrococcygeal chordomas. Int Orthop. 2006;30:514–8.
- de Bruïne FT, Kroon HM. Spinal chordoma: Radiologic features in 14 cases. AJR Am J Roentgenol. 1988;150:861–3.
[Crossref] [Google Scholar] [PubMed]
- Chandawarkar RY. Sacrococcygeal chordoma: A review of 50 consecutive patients. World J Surg. 1996;20:717–9.
[Crossref] [Google Scholar] [PubMed]
- York JE, Kaczaraj A, Abi-Said D, Fuller GN, Skibber JM, et al. Sacral chordoma: 40-year experience at a major cancer centre. Neurosurgery. 1999;44:74–9; discussion 79-80.
[Crossref] [Google Scholar] [PubMed]
- Fuchs B, Dickey ID, Yaszemski MJ, Inwards CY, Sim FH. Operative management of sacral chordoma. J Bone Joint Surg Am. 2005;87:2211–6.
[Crossref] [Google Scholar] [PubMed]
- Correia S, Dinis P, Rolo F, Lunet N. Prevalence, treatment and known risk factors of incontinence and overactive bladder in the non-institutionalized Portuguese population. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:1481–9.
[Crossref] [Google Scholar] [PubMed]
- Hulen CA, Temple HT, Fox WP, Sama AA, Green BA, et al. Oncologic and functional outcome following gastrectomy for sacral chordoma. J Bone Joint Surg Am. 2006;88:1532–9.
[Crossref] [Google Scholar] [PubMed]
- Ahmed AR. Safety margins in resection of sacral chordoma: Analysis of 18 patients. Arch Orthop Trauma Surg. 2009;129:483–7.
[Crossref] [Google Scholar] [PubMed]
- Young VA, Curtis KM, Temple HT, Eismont FJ, DeLaney TF, et al. Characteristics and Patterns of Metastatic Disease from Chordoma. Sarcoma. 2015;2015:517657.
[Crossref] [Google Scholar] [PubMed]




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.