Patients Online Registration System: Feasibility and Perceptions
2 College of Public Health and Health Informatics, PO Box 9515, 21423, Jeddah, Saudi Arabia, Email: JustiniaT@ksau-hs.edu.sa
Citation: Kedwan FH, et al. Patients Online Registration System: Feasibility and Perceptions. Ann Med Health Sci Res. 2017; 7: 90-95
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Aim: This study attempts to measure patient and Registration and Admission (R&A) staff satisfaction levels towards the Traditional Queuing Method (TQM) in comparison with a proposed Online Registration System (ORS). This study also investigates patients’ perceptions of the ORS and the feasibility and acceptance of the R&A staff in a healthcare organization. Materials and Methods: A stratified random sampling technique was used to distribute 385 questionnaires among outpatients registration area to gather indicating information and perspectives. Additionally, eleven face-to-face semi-structured interviews with front line hospital workers in the R&A department were conducted using a thematic content analysis approach to analyze the contents and produce results. In order for the researcher to have a direct understanding of the registration processes and activities and to gain a better understanding of the patients’ behaviors and attitudes toward them; a non-participant observation approach was conducted where observational encounters’ notes were taken and then analyzed. Results: It was found that most outpatient population (patients and registration staff) prefer ORS for a range of reasons including time consumption, cost benefit, patient comfort, data sensitivity, effortless, easiness, accuracy, and less errors. On the other hand, around 10% of them chose to go on with the TQM. Their reasons ranged from the unavailability of computer devices or internet connections to their educational backgrounds or physical disabilities. Computing devices and internet availability proved not to be an issue for the successful implementation of the ORS system, as most participants consented to having an internet connection or a device to enter ORS system (91%). Conclusion: Since more than half of the participated patients were unhappy with the TQM at registration desks (59.7%), this dissatisfaction should be addressed by an ORS implementaion that would reduce waiting time, enhance the level of attention, and improve services from frontline staff toward patients’ care.
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Keywords
Online Registration System (ORS); Patient registration; Health informatics; Qualitative research
Introduction
Patients’ registration is defined as the process by which a patient is diagnosed at a member institution where information is entered into the institution’s records for a selected clinical trial and then, issued for a treatment assignment. [1]
There are two accepted approaches to patient registration; either the TQM or through an ORS. [2] The satisfaction of patients and the R&A staff with the patient’s ORS have been discussed in the literature with the aim of proving the effectiveness and efficiency of this system in advanced healthcare settings.
Challenges
Even though the ORS may appear to be a constructive move towards electronic healthcare transactions, many studies have shown certain challenges against its success that should be avoided and addressed in future implementation projects or researches. [3] Such challenges include the lack of conducting internal and external marketing and advertising, educational programs, orientation posters, non-attendance occurrences, not having the capability to use the computer, lack of communication between the healthcare providers and the patients and engaging the end users. It is important to consider all of these issues for the sake of a successful system implementation and outcomes. [4,5]
Solutions
A discussion about the solutions for ORS project success suggested accomplishing further studies on various interventions such as the promotion of ORS, and the use of a reminder system [6]. Other technological solutions include direct data entry (DDE) or touch-screen computer kiosks in hospital waiting rooms. [3] These technological solutions answer and solve the problem that was raised by both Weiping et al., Coa et al., and Zhang et al. which is the lack of capability of using computers or patients whom do not have access to the internet. These studies illustrate new benefits of using the ORS such as the eligibility inquiry and response using the Health Insurance Portability and Accountability Act (HIPAA) transaction standards that was indorsed by the Senate and House of Representatives of the Congress of the United States of America in 1966.
Another solution by Short liff raises the importance of sharing the data between patients and frontline coordinators in case of vital information related to healthcare as discussed in Dent & Eason’s research. Therefore, the input from a patient through the portal could be seen from the healthcare providers’ side to be used as an input for other purposes serving the patients’ healthcare. This solution saves time of reentering the same data again and also saving money in recruiting extra clerks for this job. A study supporting this theorem is by Friedman and Wyatt in their book of evaluation methods in biomedical informatics stating that registration data connections were necessary to simplify the importing of demographic data into the system and provide data about which patients are active in the clinic at a particular time. [4] A cross sectional research by Wani and Sankaranarayanan provides an advanced solution in the mobile based appointment system. [7] This solution solved many issues in the ORS such as the ability to cancel, reschedule or the capability of reminding patients of their upcoming appointments.
Best practices
Advices toward the ORS success encourages the consideration of user co-design and participation and take their needs requirements prior to the design or implementation to have a broad perspective of the system from the end user’s point of view and also to grow the system ownership in the front-line staff who will hold the coordination processes later on whenever the patient gets lost in the system. [8] Dent and Eason argue that for the sake of a successful technical system implementation such as the ORS which will be run in a complex and advanced organization setting, the new invented system needs to be treated as a process of organizational learning in which users are given the time and space to customize their practices and needs within the capabilities of the technology used which will enhance the adoption and ownership of the new system among them.
Objectives of the study
This study measures the level of perceived satisfaction among patients toward the current TQM compared with the suggested ORS. It also investigates the patient perceptions on implementing an ORS System, and the feasibility and acceptance of the R&A staff. Additionally, this study examines the possibility of enhancing the scheduling processes, and observes the potential barriers and limitations of implementing the ORS.
At the end of this research, we would be able to answer the following questions: what is the level of perceived satisfaction among patients toward the current old fashion TQM compared to the suggested ORS? What are their perceptions on implementing an ORS System? And what is the acceptance level, constraints, and motivations of the R&A staff regarding this type of implementation?
Material and Methods
A mixed methods approach was used. Front line staff members were interviewed, and outpatients were surveyed via a crosssectional questionnaire, including non-participant observation (Appendix 1). Questionnaire results were used to extract codes that were later used as predetermined themes for the qualitative data collection steps.
Quantitative questionnaire
Stratified random sampling was applied, in which participants were randomly selected to fill up the questionnaires (Appendix 2). The total number of outpatients in the hospital up to 24/12/2014 was 2,000,000 patients, of them 54.4% were outpatients (1,087,326/2,000,000). From 1,087,326 outpatients, 385 were randomly selected to be surveyed according to the sampling calculation considering 95% level of confidence and 5% margin error.
Qualitative interviews
Face-to-face semi-structured interviews were conducted with front line hospital workers in the R&A Department using an interview guide (Appendix 3) included were 37 registration workers; 46% of them in the outpatient area (17/37). The outcomes of those interviews were analyzed using a thematic content analysis mechanism. Interviews contents were transcribed by principle investigator and co-investigator, and results of themes were compared. [9-11]
Qualitative non-participant observation
A total of 15 hours of general observations of the processes and procedures in the outpatient registration area were conducted. Being immersed in observation helped the researcher to understand and have a better perspective of the participants’ experience. [12,13]
Project design
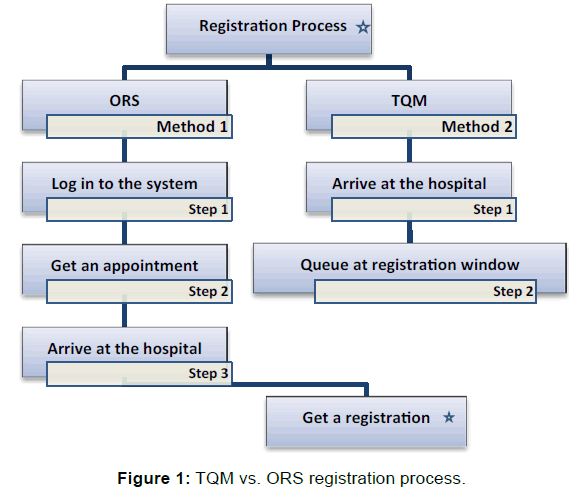
The ORS is resampled in patients who can select which consultant they prefer and which clinics they need to visit or any services provided by the hospital through the hospital portal. What a patient is going to need for an ORS is the Medical Record Number (MRN), service date and time, type of service, Personal contact information, patient’s condition (Disable, senior citizen, pregnant, infant, or normal patient), gender, and date of birth. Then, they are given an appointment number. After submission of an ORS form, the patient receives a confirmation phone message from the hospital. They will also be reminded to bring all the related materials with them on the day of their visit along with any items listed on their registration form. [14] At the designated appointment time, patients arrive at the hospital and get the registration that is chosen to their appointment number and check-in with the registration staff to sign the required consent forms (Appendix 4). These patients need not to queue at the registration window, and only need to bring their identification and medical cards at the time of service. A description of the two different approaches ORS and TQM are explained in Figure 1.
Ethical considerations
IRB approval was received from the KAIMRC research center and was registered under Research Protocol SP15/074, and all participants were consented (Appendix 5).
Internal validity
Quantitative data: Beside the registration processes validity and completeness of registration processes, [15] correct procedures were applied to assure research project internal validity as well to enable finding reliable answers to the research questions as a pre-testing (piloting) of the survey on a small group of experts were conducted prior to applying it upon outpatient participants. Accepted scientific principles of analysis methods were applied to produce reliable and unbiased data and relevant to the research questions. Quantitative results were analyzed using MS Excel calculation formulae for data that were collected from ambiguous and random participants.
Dependent variable (ORS satisfaction) was assured to be only caused by the independent variables rather than other external variables to make sure that results are valid, concise and generalizable.
Qualitative data: Qualitative data was transcribed by principle investigator and co-investigator. The 2 transcript themes were then compared to guarantee validity. The final result was decided by a unified agreement after using multiple methods to review and validate findings. [16]
External validity: Participant’s selection bias was avoided by including participants who are frequently under medical care. All participants were randomly selected to eliminate population selection bias and be representative of the general population of Saudi Arabia.
Data analysis
Quantitative data (Questionnaire): Categorical variables (age group, level of education, level of satisfaction) were presented as frequencies and percentages (Appendix 6). Coding scheme of qualitative parts in questionnaires was conducted to convert qualitative results into quantitative frequencies. Percentages of a particular category under each measurable variable are calculated by subtracting all other categories frequencies from the total number of participants (385 patients). Percentages then are compared to analyze and examine which variables have the most effect on the success or failure of ORS system implementation and which variables are against or with TQM registration process. Results and discussion of the outputs from those calculations are presented in the results section.
Qualitative data (Interview): Regarding the purposive interviews conducted to frontline staff, their outcome information was transcribed and translated whenever necessary, analyzed, and managed.
Non-participant observation: For the 15 hours of observations, a noteworthy and relevant observations were written down. General outpatient’s processes and workflow were summarized. The outcome was then analyzed and managed by the researcher using a thematic content analysis mechanism.
Result and Discussion
Quantitative questionnaire results
The collected data presented in Table 1 were analyzed to measure satisfaction and views in regard to the ORS against the TQM. ORS gained 89.1% of total votes. To investigate their perception of ORS, they were asked to explain why they chose to go with ORS. Their answers ranged from Data sensitivity (2.4%), Time consumption (16.2%), Cost benefit (4.5%), Patient comfort (23.9%), Effortless (20.7%), Easiness (27.3%), Accuracy (1.8%), Errorless (3.2%).
| SN | Category | Values | Frequency | Percentage |
|---|---|---|---|---|
| 1 | Do you have a device to enter ORS? | Yes | 352 | 91.5% |
| No | 33 | 8.5% | ||
| 2 | If yes, please specify your device. | Tablet | 45 | 11.7% |
| Smartphone | 206 | 53.5% | ||
| Laptop | 49 | 12.7% | ||
| Computer | 85 | 22.1% | ||
| 3 | Do you have internet? | Yes | 353 | 91.7% |
| No | 32 | 8.3% | ||
| 4 | When you registered in the Hospital, were you satisfied with the usual registration method at registration desk? | Very satisfied | 0 | 0% |
| Satisfied | 58 | 15.1% | ||
| Neutral | 97 | 25.2% | ||
| Dissatisfied | 169 | 43.9% | ||
| Very Dissatisfied | 61 | 15.8% | ||
| 5 | How long does it take you to finalize your registration process, from queuing on registration window until you see a physician? | 15 min or less | 0 | 0% |
| 16 - 20 min | 33 | 8.6% | ||
| 21 - 30 min | 108 | 28.1% | ||
| 31 - 40 min | 193 | 50.1% | ||
| 41 min or Above | 51 | 13.2% | ||
| 6 | Are you satisfied with the level of attention and service you get from frontline staff? | Very satisfied | 0 | 0% |
| Satisfied | 54 | 14% | ||
| Neutral | 163 | 42.3% | ||
| Dissatisfied | 121 | 31.4% | ||
| Very Dissatisfied | 47 | 12.3% | ||
| 7 | Which one do you prefer? | Hospital ORS | 343 | 89.1% |
| Hospital queuing registration | 42 | 10.9% | ||
| 8 | If your answer is number 1, why do you think ORS is efficient? | Data sensitivity | 32 | 2.4% |
| Time consumption | 220 | 16.2% | ||
| Cost benefit | 63 | 4.5% | ||
| Patient comfort | 324 | 23.9% | ||
| Effortless | 281 | 20.7% | ||
| Easiness | 371 | 27.3% | ||
| Accuracy | 24 | 1.8% | ||
| Errorless | 43 | 3.2% | ||
| 9 | If your answer is number 2, what is your reason for not wanting to use the ORS? | No internet | 32 | 31.4% |
| No device to enter ORS | 33 | 32.4% | ||
| Educational Issues | 25 | 24.5% | ||
| Physical Disability | 12 | 11.7% | ||
| 10 | If you can use ORS, what do you prefer? | Register from home | 305 | 79.2% |
| Register from hospital kiosks | 51 | 13.3% | ||
| Register from registration desk | 29 | 7.5% | ||
| 11 | What is your level of education? | Primary or less | 26 | 6.8% |
| Elementary | 56 | 14.5% | ||
| Secondary | 192 | 49.9% | ||
| Bachelor | 98 | 25.5% | ||
| Master or above | 13 | 3.3% | ||
| 12 | How old are you? | 0 - 20 years old | 4 | 1% |
| 21 - 30 years old | 98 | 25.5% | ||
| 31 - 40 years old | 139 | 36.1% | ||
| 41 - 50 years old | 96 | 24.9% | ||
| 51 - Above | 48 | 12.5% |
Table 1: Quantitative data presentation.
From those statistics, we understand that their biggest concern is the easiness of using the ORS system compared to the effort spent in coming to hospitals, queuing for hours to get screened or given the kind of service they are after. To have a comfortable treatment environment and the ability to book for appointments or register from home effortlessly comes as a second goal (79.2%). It is also important to notice that most patients were unaware of the main goal of ORS which is data sensitivity, accuracy, and it’s potentiality of being error-free. Contrariwise, TQM voters (10.9%) were also asked for their motives. Their reasons were the unavailability of computer devices (32.4%) or internet connections (31.4%), besides educational background (24.5%) and physical disabilities (11.7%). Noticably, their refusal of the ORS is not mainly because of any defects in ORS itself, but rather to other probable economic or educational issues.
Computing devices and internet availability have proved to be not an issue for the successful implementation of the ORS as most of patients have consented to have both (91.5%, 91.7% respectively) whether the device is a tablet, smart phone, laptop, or a computer.
More than half of patients were unhappy with the usual registration method at registration desks (59.7%). This percentage doesn’t indicate how much patients are indeed unsatisfied as quarter of them voted for neutral which might be because they were unable to judge, possibly because they havn’t tried ORS yet to have a better understanding of what they are being asked about. Another possible reason for their dissatisfaction could be related to the amount of waiting time they have to tolerate per visit.
Patients were asked whether they are satisfied with the level of attention and service they get from frontline staff, only 14% of them said they are satisfied. This is a big indication that staffs are too overwhelmed with their daily routine duties instead of assuring patients comfort, guidance, and good care.
Patients’ demographics could also be possible reasons of ORS failure or refusal as more than 12% of patients were above 51 years old and more than 21% held elementary certificates or lower. Even though there are elderly patients who are highly educated (possibly 3.3%), this can still be taken as a reasoning factor behind the inability to cooperate with ORS.
This quantitative study gave us a general perspective of the potencial reasons behind patient’s perception and cooperation levels regarding the use of ORS.
Qualitative interview results
Predetermined themes were derived from the questionnaires and used to conduct purposive interviews with the outpatient registration staff (Appendix 7). Interviews were summarised in a table to analyse only highly relevant statements (Appendix 8). To some extent, time factor, cost benefit, crowded environment, health related issues, patient’s educational background, hard\ software availability, privacy and security concerns, higher management involvement, and age group had a direct impact on registration staff’s perspective and acceptance toward ORS system implementation.
Weiping et al. explained how front line hospital employees are often times-overwhelmed, besides the necessity of building a good relationship with the patients for more service satisfaction. [7] Through the non-participant observations, live as they happen, the researcher noticed an event acts as an indicator to the sressful atmosphere for both frontline staff and patients resulted in an aggresseive and unprofessional scene.
“There is a male with his wife shouting with the registration staff at the window about how long have they been waiting and the reason behind the delay. She (the registration staff) became angry and responded aggressively that this is how things work and then she left the station for 15 minutes to calm down” (Day 3 (18/8/2015), 10:15 – 10:36)
As the hospital receives up to 500 patients a day and over 1 million patients, it would take almost all of the employee’s time and effort to control and guide those continuous streams of patients.
Amatayakul believes that long waiting times of registration to see a healthcare provider is problematic and reductions in waiting times for medical services could help promote patients’ satisfaction. [17]
As a major goal, the hospital aims to maintain patient’s satisfaction at all times in epidemiological conditions or healthy seasons.
“I strongly agree on the necessity to move forward and adopt the ORS because it would eliminate lots of unnecessary routine work. I support ORS because the input from patient through the portal (e-services) could be seen by the registration staff side to be used as an input for other purposes serving the patients’ healthcare services and saving a lot of time that was used previously for data entry.” (Reg. junior staff 6)
Shortliffe raises the importance of sharing the data between patients and frontline coordinators in case of vital information related to healthcare as discussed in Dent & Eason’s research. [2] ORS is believed to be a solution that saves time and money in recruiting extra clerks for which causes unnecessary expenditures.
Besides the dangerous potential hazards in case of any infectious diseases distribution among outpatients occupying the whole outpatient area especially with the existence of children. Below are two observations supporting these statements?
“There are 4 mothers with their children waiting in the area, 2 of those children are infants.” (Day 2 (17/8/2015), 9:18 – 9:30 a.m.)
“I heare patients snease and couph continuously as per their arrival. Apparantly they have got influenza.” (Day 2 (17/8/2015), 10:26 – 10:35 a.m.)
Weiping et al. thinks that the major ORS limitation is the lack of conducting adequate advertising. [7]
“I would suggest ideas such as clear and simple brochures with big fonts describing ORS in few words for a beginning, and in the second stage, a more teaching concepts be adopted.” (Reg. junior staff 3)
Since most of military hospital patients are from a limited educational background according to the nature of the hospital recruitment requirements and skills. It is believed that this factor would be fatal in the ORS implementation life cycle.
“We have distributed boxes of user manuals; only 30% of patients actually used them. That’s why i don’t believe posters and advertising or knowledge distribution campaigns will work.” (Reg. junior staff 1)
Even though some patients are used to be served at the point of visit, still, age is not considered a crucial turning point in the ORS life cycle.
“I think old, uneducated, and some educated type of patients prefer to be served rather than be initiative and self-dependent when coming to health services.” (Reg. senior staff 1)
Zhang et al. considers the absence of internet connectivity or not having a computer device would lead to the lack of communication between healthcare providers and patients. [18]
“I am a bit anxious about the ORS idea because of the hacking risk of patients’ information as the online access could threaten patient’s safety and privacy.” (Reg. junior staff 4)
ORS encounters security threats in cloud which is used to store the patient’s information which plays a big role in withdrawing ORS one step backward making TQM a more secured method of registration. Possible strategies to improve ORS weaknesses of privacy hacking or identity thefts are to adopt highly secured firewalls or protection techniques.
These results’ outcomes clarify how and through what possible mechanisms ORS system implementation can come to positive conclusions in a cultural and sociological manners in the medical environment.
Conclusion
Health informatics has become an important component in healthcare fields. [19] It is growing swiftly, and is involved in every health care delivery aspect. [20] The emergence of informatics in the healthcare field is causing rapid advances in the way healthcare is delivered technologically. [21]
One essential area of health informatics that does not always receive enough attention is the scheduling process. It might look like a simple step with no remarkable impact on the organizations’ workflow, but by analyzing current registration processes and utilizing health informatics solutions, the workflow will ease significantly according to Dent & Eason’s research. [6]
An informatics solution can be utilized by automating the scheduling process where it can be provided online through the organizations’ portal. Not only to schedule a date and time, but the desired services as well with the payment of part or all of the fees to business center in order to allow the front-line employees to finally be more sophisticated around revenue cycle, customer service, and even financial planning.
ORS has proved to improve the workflow, lessen patient’s waiting time, and enhance patient’s care. The current registration method in the hospital is the old traditional method of queueing and waiting for 2 to 3 hours to actually see the healthcare providers. The waiting time in a very crowded waiting area frustrates the patients leading to their dissatisfaction.
Since there is no ORS implemented in any way in the hospital’s current website portal, the results of this study justify the main objectives by proving that more than half of patients were unhappy with the TQM at registration desks (59.7%) This dissatisfaction should be addressed by ORS implementaion that would reduce waiting time, enhance the level of attention and service from frontline staff toward patients’ care.
Acknowledgement
Besides my supervisor Dr. Taghreed Justinia, I would like to mention that his research was supported by the College of Public Health and Health Informatics and the King Abdullah International Medical Research Centre. I am also thankful to the University of King Saud Bin Abdulaziz University for Health Sciences and every faculty member who participated in my educational process.
Conflict of Interest
There are no conflicts of interest to report.
REFERENCES
- Herson J. Patient registration in a cooperative oncology group. Controlled Clinical Trials, 1980; 1: 101-110.
- Shortliffe E. Biomedical informatics: Computer applications in health care and biomedicine (3rd ed., p. 1060). New York, NY: Springer, 2006.
- Amatayakul M. Electronic health records: A practical guide for professionals and organizations (5th ed.). Chicago, Ill.: AHIMA, 2013.
- Friedman C, Wyatt J. Evaluation methods in medical informatics (2nd edn). New York: Springer, 2006.
- Coa W, Wan Y, Tu H, Shang F, Lie D, Tan Z, et al. A web-based appointment system to reduce waiting for outpatients: A retrospective study. BMC Health Services Research, 2011; 11: 318
- Act A.. Health insurance portability and accountability act of 1996. Public Law, 104, 191, 1996.
- Dent M, Eason K. Electronic information in health and social care-promises and pitfalls. Health Informatics Journal, 2014; 20: 165-167.
- Weiping YU, Xiaowen YU, Hao HU, Guimin DU, Liu Z, Wang Y. Use of Hospital Appointment Registration Systems in China: A Survey Study. Global Journal of Health Science, 2013; 5: 193.
- Bowen GA. Document analysis as a qualitative research method. Qualitative research journal, 2009; 9: 27-40.
- Zhang M, Zhang C, Sun Q, Cai Q, Yang H, Zhang Y. Questionnaire survey about use of an online appointment booking system in one large tertiary public hospital outpatient service center in China, 2014.
- Levine DM, Berenson ML, Stephan D. Statistics for managers using Microsoft Excel (Vol. 660). Upper Saddle River, NJ: Prentice Hall, 1999.
- Vinten G. Participant observation: A model for organizational investigation?. Journal of Managerial Psychology, 1994; 9: 30-38.
- Wani SMA, Sankaranarayanan S. Intelligent mobile hospital appointment scheduling and medicine collection, 2014.
- Weiss RS. Learning from strangers: The art and method of qualitative interview studies. Simon and Schuster, 1995.
- Turner DW. Qualitative interview design: A practical guide for novice investigators. The qualitative report, 2010; 15: 754-760.
- Yates F. Sampling methods for censuses and surveys. Sampling methods for censuses and surveys, 1949.
- Hommel K, Rasmussen S, Madsen M, Kamper AL. The Danish Registry on Regular Dialysis and Transplantation: completeness and validity of incident patient registration. Nephrology Dialysis Transplantation, 2010; 25: 947-951.
- McDermott R. Internal and external validity. Cambridge handbook of experimental political science, 2011; 27-40.
- Oliver GR, Hart SN, Klee EW. Bioinformatics for Clinical Next Generation Sequencing. Clinical chemistry, 2015; 61: 124-135.
- Feuerstein M, Wildhirt SM, Bauernschmitt R, Navab N. Automatic patient registration for port placement in minimally invasixe endoscopic surgery." Medical Image Computing and Computer-Assisted Intervention–MICCAI. Springer Berlin Heidelberg, 2005; 287-294.
- Chen H. Medical informatics knowledge management and data mining in biomedicine. New York, NY, USA, Springer, 2005.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.